Odyssey outcomes - elderly patients results
Odyssey Outcomes: Addition of PCSK9i to background Statin therapy further reduces MACE.
Elderly patients sub-analysis overview
Study outcomes
Primary outcome: composite of death from CHD, nonfatal myocardial infarction, fatal or nonfatal ischemic stroke, or unstable angina requiring hospitalization
Key secondary outcome: all-cause death
All outcomes were adjudicated by physicians who were unaware of the trial-group assignments
*Pre-specified analysis: Age <65 years (n=13,840), age≥65 years (n=5,084). The Cox regression model with age as a continuous variable, randomized treatment and the interaction was used to estimate the event rate at 3 years and HRs comparing alirocumab versus placebo at specific ages to test the interaction between age and treatment with alirocumab
Baseline characteristics by age group
|
Characteristic |
<65 years (n=13,840) |
≥65 years (n=5084) |
P-value |
|
Age (years), mean ± SD |
54.2 ± 6.3 |
70.5 ± 4.7 |
|
|
Women, n (%) |
2948 (21.3) |
1814 (35.7) |
<0.0001 |
|
Medical history before index ACS, n (%) |
|
|
|
|
Hypertension |
8390 (60.6) |
3859 (75.9) |
<0.0001 |
|
Diabetes mellitus |
3787 (27.4) |
1657 (32.6) |
<0.0001 |
|
Myocardial infarction |
2499 (18.1) |
1134 (22.3) |
<0.0001 |
|
Percutaneous coronary intervention |
2212 (16.0) |
1029 (20.2) |
<0.0001 |
|
Coronary artery bypass graft |
582 (4.2) |
465 (9.1) |
<0.0001 |
|
Stroke |
337 (2.4) |
274 (5.4) |
<0.0001 |
|
Peripheral artery disease |
428 (3.1) |
331 (6.5) |
<0.0001 |
|
Congestive heart failure |
1800 (13.0) |
1014 (19.9) |
<0.0001 |
|
Index, ACS, n (%) |
n=13,818 |
n=5075 |
<0.0001 |
|
STEMI |
5039 (36.4) |
1497 (29.4) |
|
|
Non-STEMI |
6422 (46.4) |
2753 (54.2) |
|
|
Unstable angina |
2357 (17.0) |
825 (16.2) |
|
|
PCI or CABG for index ACS, n (%) |
10,201 (73.7) |
3475 (68.4) |
<0.0001 |
SD, Standard deviation
|
Characteristic |
<65 years (n=13,840) |
≥65 years (n=5084) |
P-value |
|
The from index ACS to randomization |
3.6 ± 2.8 |
3.8 ± 2.8 |
0.0003 |
|
Body mass index (kg/m2), mean ± SD |
28.8 ± 4.9 |
27.8 ± 4.6 |
<0.0001 |
|
Renal function |
|
|
|
|
eGFR (mL/min), mean ± SD |
83.1 ± 18.5 |
70.2 ± 18.2 |
<0.0001 |
|
eGFR <60 mL/min, n (%) |
1,163 (8.4) |
1,377 (27.1) |
<0.0001 |
|
Lipid-lowering drugs at randomization, n (%) |
|
|
<0.0001 |
|
High-intensity |
12,565 (90.8) |
4,246 (83.5) |
|
|
Low- or moderate-intensity atorvastatin/rosuvastatin |
1,027 (7.4) |
580 (11.4) |
|
|
No statin |
222 (1.6) |
238 (4.7) |
|
|
Ezetibime |
408 (2.9) |
142 (2.8) |
0.57 |
eGFR, estimated glomerular filtration rate
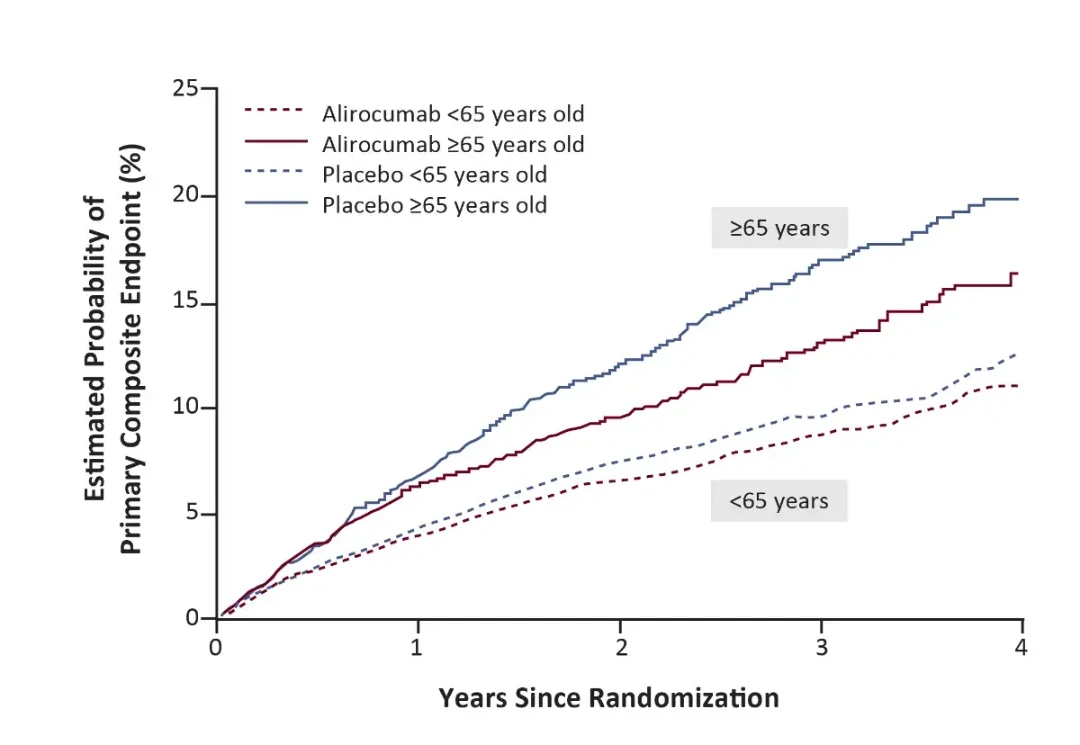
Treatment effect by age group: Primary composite outcome
Relative Risk Reduction Hazard Ratio (Alirocumab vs Placebo)
≥65 years: 0.78, 95% CI 0.68-0.91
<65 years: 0.89, 95% CI 0.80-1.00
Interaction p-value: 0.19
Absolute Risk Reduction At 3 years (Placebo - Alirocumab)
≥65 years: 3.88%, 95% Cl 1.74-6.02
<65 years: 0.91%, 95% Cl -0.13 to 1.95
Interaction p-value: 0.015
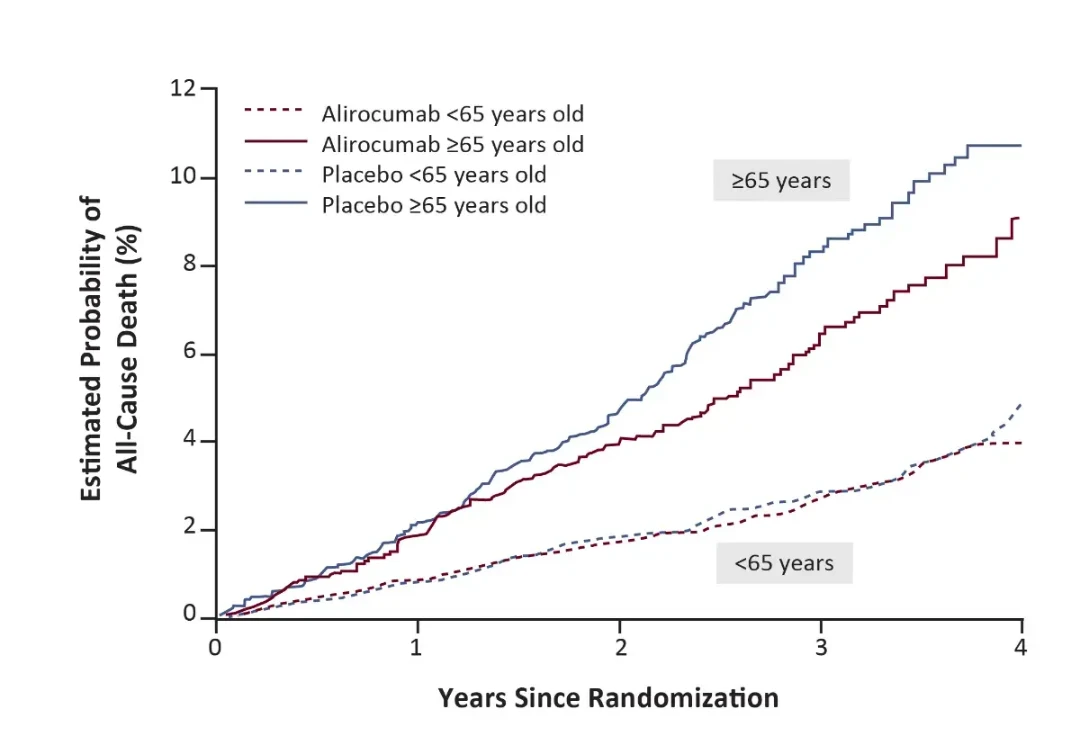
Treatment effect by age group: All cause death
Relative Risk Reduction Hazard Ratio (Alirocumab vs Placebo)
≥65 years: 0.77, 95% CI 0.62-0.95
<65 years: 0.94, 95% CI 0.77-1.15
Interaction p-value: 0.46
Absolute Risk Reduction At 3 years (Placebo - Alirocumab)
≥65 years: 2.08%, 95% Cl 0.48-3.67
<65 years: 0.11%, 95% Cl -0.50 to 1.72
Interaction p-value: 0.024
Safety: Adverse events by age group
|
Adverse Event |
Randomized Treatment |
Relative Risk (95%CI) Alirocumab vs Placebo |
|
|
|
Alirocumab, N (%) |
Placebo, N (%) |
|
|
Any adverse event |
|
|
|
|
≥65 years |
1,974 (79.0) |
2,042 (79.3) |
1.00 (0.97 -1.02) |
|
<65 years |
5,191 (74.7) |
5,240 (76.3) |
0.98 (0.96 -1.00) |
|
Serious adverse event |
|
|
|
|
≥65 years |
703 (28.1) |
781 (30.3) |
0.93 (0.85 -1.01) |
|
<65 years |
1,499 (21.6) |
1,569 (22.8) |
0.94 (0.89 -1.00) |
|
Adverse event leading to discontinuation of treatment |
|
|
|
|
≥65 years |
121 (4.8) |
128 (5.0) |
0.97 (0.76 -1.24) |
|
<65 years |
222 (3.2) |
196 (2.9) |
1.12 (0.93 -1.35) |
|
Neurocognitive disorder |
|
|
|
|
≥65 years |
52 (2.1) |
65 (2.5) |
0.82 (0.57 -1.18) |
|
<65 years |
91 (1.3) |
102 (1.5) |
0.88 (0.67 -1.17) |
|
New-onset diabetes in patients w/o diabetes at baseline |
|
|
|
|
≥65 years |
156 (9.2) |
167 (9.7) |
0.95 (0.77 -1.17) |
|
<65 years |
492 (9.7) |
509 (10.2) |
0.95 (0.84 -1.07) |
|
Hemorrhagic stroke - adjudicated |
|
|
|
|
≥65 years |
1 (0.0) |
6 (0.2) |
0.17 (0.02 -1.42) |
|
<65 years |
8 (0.1) |
10 (0.1) |
0.79 (0.31 -2.00) |
|
Alanine aminotransferase> 3 x upper limit of normal |
|
|
|
|
≥65 years |
64 (2.6) |
70 (2.8) |
0.94 (0.67 -1.31) |
|
<65 years |
148 (2.1) |
158 (2.3) |
0.92 (0.74 -1.15) |
|
Aspartate |
|
|
|
|
≥65 years |
52 (2.1) |
48 (1.9) |
1.11 (0.75 -1.64) |
|
<65 years |
108 (1.6) |
118 (1.7) |
0.90 (0.70 -1.17) |
Elderly Patients’ sub-analysis conclusions¹
- Alirocumab demonstrated an effective RRR for primary MACE outcome, and was associated with an effective reduction of all-cause death across age categories
- There was a highly significant interaction of treatment effect and age on the absolute reduction of all-cause death, and although adverse events generally were more frequent in older patients, there was no increase occurrence in any of the safety endpoints
SD, Standard deviation
- Sinnaeve PR, et al. Eur Heart J. 2020; 41(24):2248-58