Chronic Spontaneous Urticaria is an Immune-Mediated Inflammatory Skin Disease
CSU IS AN IMMUNE-MEDIATED INFLAMMATORY SKIN DISEASE
CSU is characterized by the following:
Spontaneous appearance of wheals and/or angioedema that recur for 6 weeks or more, occurring on most days of the week1–4
 |
Wheals2,5
Angioedema2–6
|
 |
Chronicity7–9 The average duration of CSU is reported as 1–5 years, but may be longer in more severe cases |
 |
Intense itch1,2,4 TPatients rate itch as the most bothersome symptom of CSU7 |
 |
Significant burden on quality of life: |
 Sleep disturbance5*,10**
Sleep disturbance5*,10**
Most people with CSU (92%) experience sleep problems
 Appearance5*,10**
Appearance5*,10**
People with CSU ‘sometimes’ or ‘always’ feel:
Self-conscious and embarrassed (75%)
Less attractive than they used to (68%)
 Social interactions5*,10**,11
Social interactions5*,10**,11
People with CSU often report that their disease leads to:
Interference with sexual relationships (73%)
Avoidance of other people (51%)
Withdrawal from social activities (63%)
Decreased work productivity and increased absenteeism
 Mental health12†,13*‡
Mental health12†,13*‡
The most common mental health disorders among patients with CSU are:
Anxiety disorders (31%)
Mood disorders (29%)
Traumatic and stress-related disorders (17%)
CSU, chronic spontaneous urticaria.
*Study pertains to patients with chronic urticaria
**In ASSURE-CSU study with 673 CSU patients
†In a survey of 2,579 dermatology patients
‡A systematic review and meta-analysis
- Magerl M, et al. Allergy. 2016;71(6):780–802;
- Saini SS. Immunol Allergy Clin North Am. 2014;34(1):33–52;
- Radonjic-Hoesli, et al. Clin Rev Allergy Immunol. 2018;54(1):88–101;
- Zuberbier T, et al. Allergy. 2018;73(7):1393–1414;
- O’Donnell BF. Immunol Allergy Clin North Am. 2014;34(1):89–104;
- Sussman G, et al. Allergy. 2018;73(8):1724–1734;
- Maurer M, et al. Allergy. 2011;66(3):317–330;
- Kim YS, et al. Allergy Asthma Immunol Res. 2018;10(1):83-87;
- Gaig P, et al. J Investig Allergol Clin Immunol. 2004;14(3):214–220;
- Maurer M, et al. Allergy. 2017;72(5):2005–2016;
- Balp MM, et al. Patient. 2015;8551–8;
- Picardi A. Br J Dermatol. 2000;143(5):983–991;
- Konstantinou GN. Clin Transl Allergy. 2019,23;42(9);1–12.
CSU LEADS TO LONG-TERM PATIENT BURDEN1-3
Who is affected by CSU?
.png) Global prevalence of
Global prevalence of
CSU is 0.5–1%4,5
.png) Most patients diagnosed
Most patients diagnosed
are 20–40 years old4
.png) CSU is more common in
CSU is more common in
adults than in children6
.png) Twice as many women
Twice as many women
are affected as men4,7
CSU, chronic spontaneous urticaria.
- Kim YS, et al. Allergy Asthma Immunol Res. 2018;10(1):83–87;
- Gaig P, et al. J Investig Allergol Clin Immunol. 2004;14(3):214– 220;
- Maurer M, et al. Allergy. 2017;72(5):2005–2016;
- Maurer M, et al. Allergy. 2011;66(3):317–330;
- Maxim E, et al. J Am Acad Dermatol. 2018;79(3):567–569;
- Anita C, et al. J Am Acad Dermatol. 2018;79(4):599–614;
- Cassano N, et al. G Ital Dermatol Venereol. 2016;151(5):544–552.
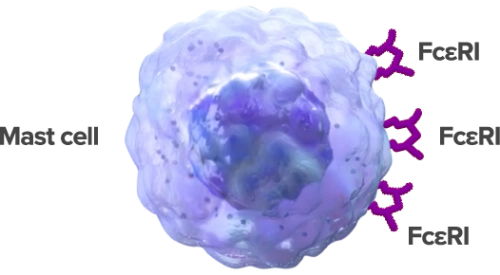
CSU IS A MAST CELL-DRIVEN DISEASE, THAT MAY BE INFLUENCED BY A DYSREGULATED TYPE 2 IMMUNE RESPONSE
The pathophysiology of CSU is not completely clear, but it is known that mast cells and their degranulation are central1…
 Mast cell
Mast cell
...and elements of the type 2 immune response are involved.1 These include:2,3
 Eosinophil Eosinophil |
 Basophil Basophil |
 Th2 cell Th2 cell |
 ILC2 ILC2 |
…and signaling mediators, notably IgE, IgG, and type 2 cytokines4–7
 IgE IgE |
 IgG IgG |
 IL-4 IL-4 |
 IL-13 IL-13 |
 IL-5 IL-5 |
 IL-31 IL-31 |
 Histamine Histamine |
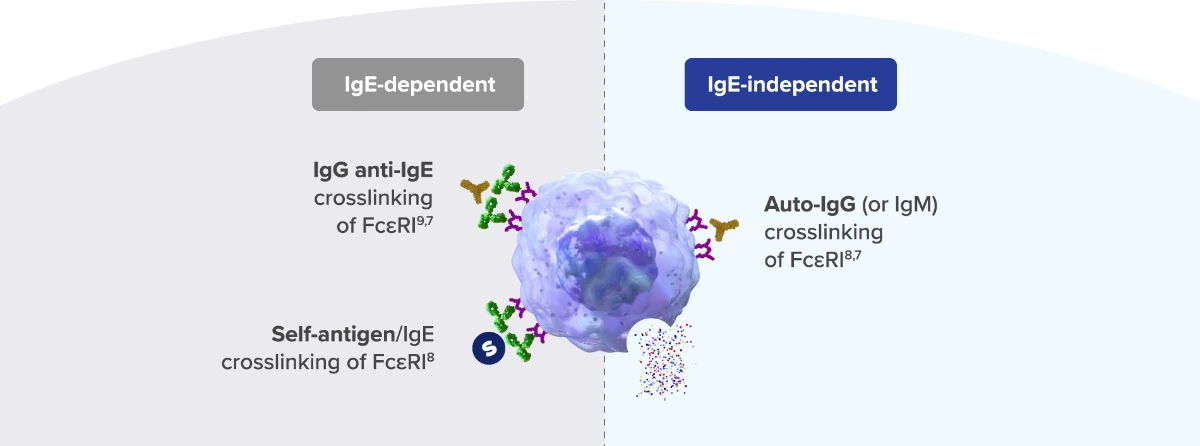
There is heterogeneity in the mechanisms triggering mast cell degranulation
Mast cell degranulation can occur via different mechanisms:*
 IgG IgG |
 IgE IgE |
 Inflammatory mediators Inflammatory mediators |
 FcεRI FcεRI |
 Self-antigen Self-antigen |
*These mechanisms may also be characterized as autoimmune/type IIb (IgG anti-IgE/IgG anti-FcɛRI) or autoallergic/type I (IgE to self-antigens).
CSU, chronic spontaneous urticaria; FcεRI, fragment constant (of Ig) receptor; Ig, immunoglobulin; IL, interleukin; ILC, innate lymphoid cell; Th2, T helper 2
CSU LEADS TO LONG-TERM PATIENT BURDEN1-3
Who is affected by CSU?
.png) Global prevalence of
Global prevalence of
CSU is 0.5–1%4,5
.png) Most patients diagnosed
Most patients diagnosed
are 20–40 years old4
.png) CSU is more common in
CSU is more common in
adults than in children6
.png) Twice as many women
Twice as many women
are affected as men4,7
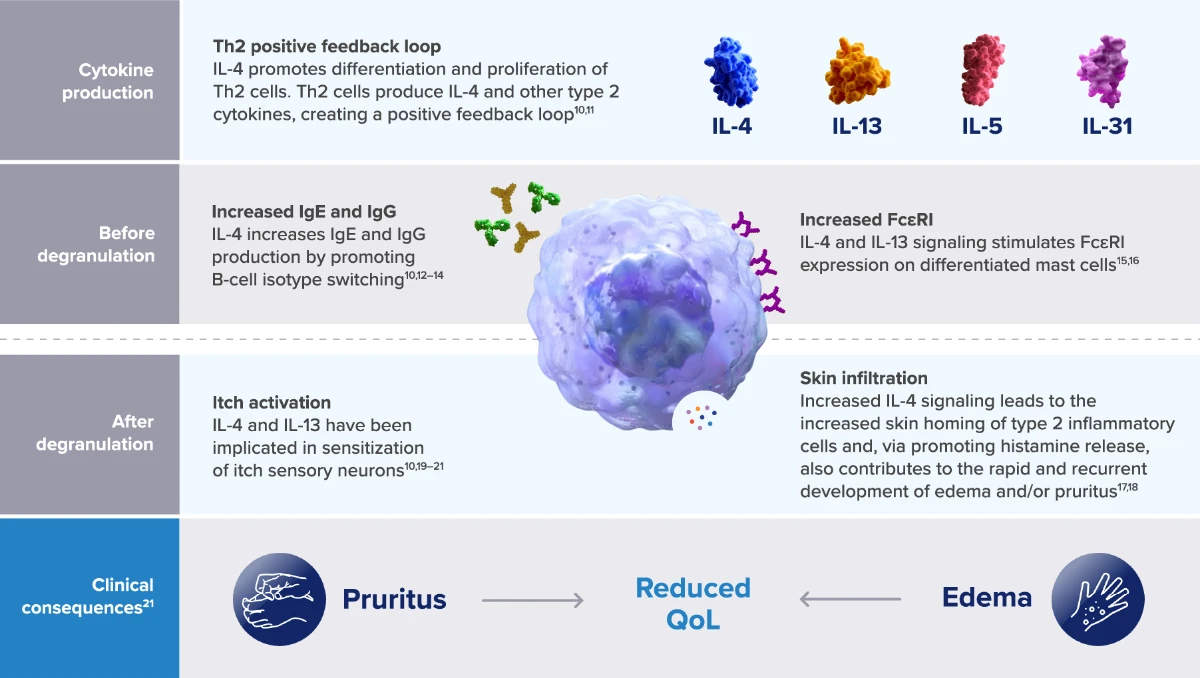
Multiple aspects of mast cell activity may be influenced by type 2 cytokines
 IgG IgG |
 IgE IgE |
 Inflammatory mediators Inflammatory mediators |
 FcεRI FcεRI |
*These mechanisms may also be characterized as autoimmune/type IIb (IgG anti-IgE/IgG anti-FcɛRI) or autoallergic/type I (IgE to self-antigens).
CSU, chronic spontaneous urticaria; FcεRI, fragment constant (of Ig) receptor; Ig, immunoglobulin; IL, interleukin; Th2, T helper 2
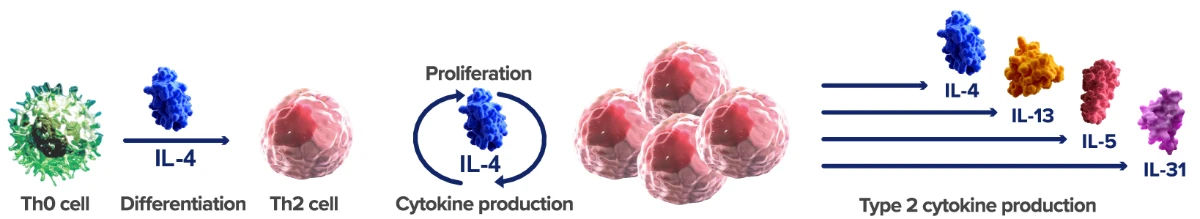
IL-4 production contributes to the type 2 inflammatory response
IL-4 promotes the differentiation of Th0 cells into Th2 cells. These Th2 cells then proliferate in response to IL-4 and produce more IL-4, along with other type 2 cytokines, in a positive feedback loop11,10
Type 2 cytokines support mast cell priming4,5
and may contribute to disease features of CSU6–10
*These mechanisms may also be characterized as autoimmune/type IIb (IgG anti-IgE/IgG anti-FcɛRI) or autoallergic/type I (IgE to self-antigens).
CSU, chronic spontaneous urticaria; FcεRI, fragment constant (of Ig) receptor; Ig, immunoglobulin; IL, interleukin; Th2, T helper 2
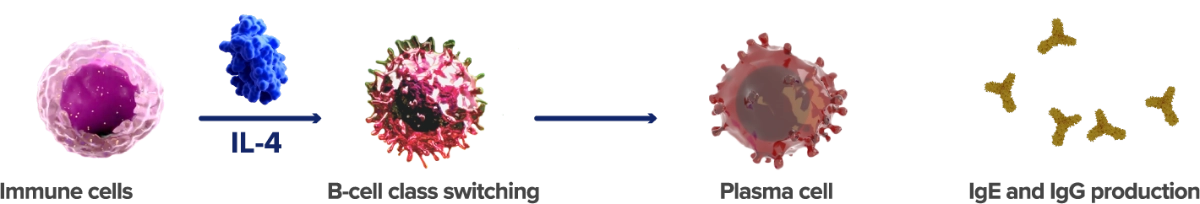
Before degranulation, IL-4 and IL-13 prime mast cells
Type 2 cells, including Th2 cells, basophils, and mast cells, produce IL-4, which drives B-cell class switching.12,13 This leads to IgE and IgG production, which is needed for IgE-dependent and IgE independent degranulation of mast cells8
IL-4 and IL-13 increase IgE receptor (FcεRI) expression, priming mast cells for degranulation15,16
*These mechanisms may also be characterized as autoimmune/type IIb (IgG anti-IgE/IgG anti-FcɛRI) or autoallergic/type I (IgE to self-antigens).
CSU, chronic spontaneous urticaria; FcεRI, fragment constant (of Ig) receptor; Ig, immunoglobulin; IL, interleukin; Th2, T helper 2
After the degranulation of mast cells, IL-4 and IL-13 have broad effects on itch and edema
| Inflammatory mediators promote immune cell infiltration | Basophils and eosinophils also contribute to CSU | ||
 |
Histamine and other inflammatory mediators cause vasodilation and increased vascular permeability, thereby promoting plasma extravasation23,24 |  |
IL-4 contributes to survival of, and FcεR1 expression by, basophils;28 these cells may have a similar role to mast cells in CSU9 |
| Increased IL-4 signaling can lead to increased skin homing of type 2 inflammatory cells, through VCAM-1 upregulation17 These may lead to the development of edema and pruritus and contribute to disease chronicity22 |
 |
Eosinophils, regulated mainly by IL-5,26 may stimulate mast cell histamine release thereby contributing to edema and itch18 | |
|
IL-4 and IL-13 are implicated in activating itch sensory pathways
|
Together, edema and itch lead to reduced patient QoL22
*These mechanisms may also be characterized as autoimmune/type IIb (IgG anti-IgE/IgG anti-FcɛRI) or autoallergic/type I (IgE to self-antigens).
CSU, chronic spontaneous urticaria; FcεRI, fragment constant (of Ig) receptor; Ig, immunoglobulin; IL, interleukin; Th2, T helper 2
- Kocatürk E, et al. Clin Transl Allergy. 2017;7:1; Erratum in: Clin Transl Allergy. 2017;3(7):11;
- Ying S, et al. J Allergy Clin Immunol. 2002;109(4):694–700;
- Wang SH and Zuo YG. Front Immunol. 2021;12:698522;
- Hide M,et al. N Engl J Med. 1993;328(22):1599–604;
- Kikuchi Y and Kaplan AP. J Allergy Clin Immunol. 2002;109(1):114–8;
- Ferrer M, et al. Int Arch Allergy Immunol. 2002;129(3):254–60;
- Caproni M, et al. J Dermatol Sci. 2004;36(1):57–9;
- Maurer M, et al. Int Arch Allergy Immunol. 2020;181(5):321– 333;
- Bracken SJ, et al. Front Immunol. 2019;10:627;
- Keegan AD et al. Fac Rev. 2021;10:71;
- Stott B, et al. J Allergy Clin Immunol. 2013 Aug;132(2):446–54.e5;
- Brown MA, et al. Cell. 1987; 50(5):809–18;
- Kondo Y, et al. Int Immunol. 2008 ;20(6):791–800;
- Bergstedt-Lindqvist S, et al. Eur J Immunol. 1988;18(7):1073–7;
- Kaur D, et al. Allergy. 2006;61(9):1047–53;
- Toru H, et al. Int Immunol. 1996;8(9):1367–73;
- Cheng LE, et al. J Exp Med. 2015; 212(4):513–24;
- Altrichter S, et al. J Allergy Clin Immunol. 2020;145(6):1510–6l;
- Bilsborough J, et al. J Allergy Clin Immunol. 2006;117(2):418–25;
- Oetjen L, et al. Cell. 2017;171(1):217–228;
- Edukulla R, et al. J Biol Chem. 2015;29(21)0:13510–13520;
- Maurer M, et al. Allergy. 2017;72(5):2005–16;
- Ashina K, et al. PLoS One. 2015; 10(7): e0132367;
- Ohtsu H, et al. Eur J. Immunol. 2002.32:1698–1708;
- Reinhart and Kaufmann. Cell Death Dis 2018.9(7):713;
- Spencer LA and Weller PF. Immunol Cell Biol. 2010;88(3): 250–6.
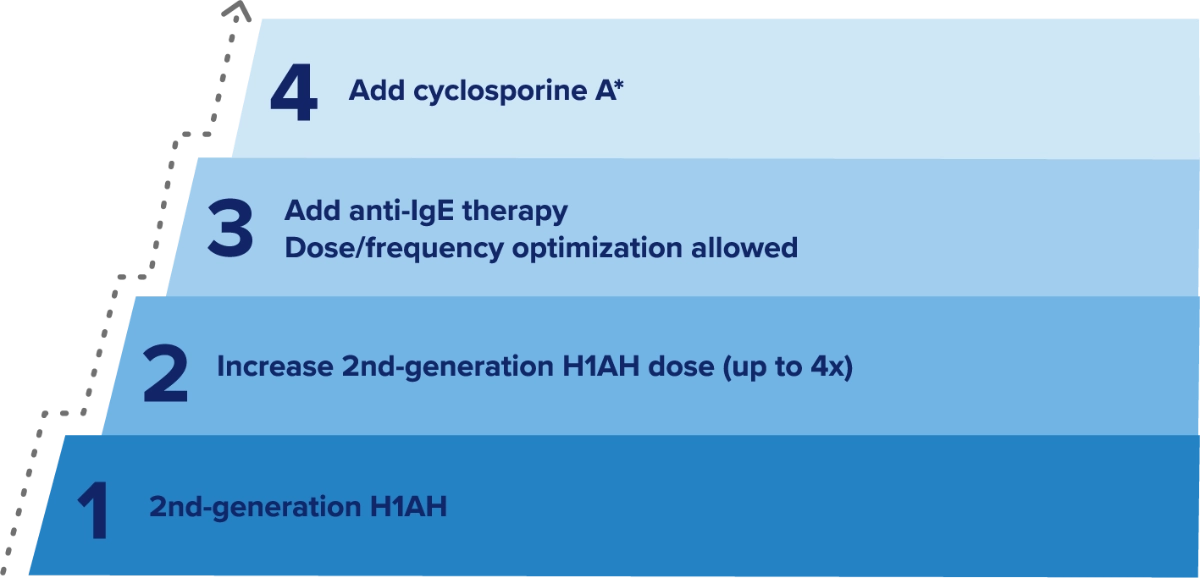
CSU TREATMENT SHOULD CONTROL DISEASE SIGNS AND SYMPTOMS
The aim of CSU treatment is to improve patient quality of life through1,2:
 Controlling signs and symptoms of CSU Controlling signs and symptoms of CSU |
 Therapies with a favorable safety and tolerability profile Therapies with a favorable safety and tolerability profile |
EAACI/EDF treatment guidelines recommend a four-step approach to treatment1,2
Type 2 mediators beyond IgE may be therapeutic targets for CSU
Despite the use of antihistamines and anti-IgE treatments, some patients are not adequately controlled.3-5
More advanced and specific targeted therapies are needed for safe and effective treatment of these patients
Type 2 inflammation has been suggested to play a role in the disease features and underlying mechanisms of CSU6–8
*As an alternative to anti-IgE therapy
CSU, chronic spontaneous urticaria; EAACI, European Academy of Allergology and Clinical Immunology; EDF, European Dermatology Forum; H1AH; histamine 1 receptor antihistamine; Ig, immunoglobulin.
- Zuberbier T, et al. Allergy. 2021;77(3):734–766;
- Bernstein J, et al. J Allergy Clin Immunol. 2014;133(5):1270–1277;
- Guillén-Aguinaga S, et al. Br J Dermatol. 2016;175(6):1153–1165;
- Min TK and Saini SS. Allergy Asthma Immunol Res. 2019;11(4):470–481;
- Kolkhir P, et al. Ann Allergy Asthma Immunol. 2020;124(1):2–12;
- Caproni M, et al. J Dermatol Sci. 2004;36(1):57–59;
- Cevikbas F, et al. J Allergy Clin Immunol. 2014;133(2):448–460;
- Feld M, et al. J Allergy Clin Immunol. 2016;138(2):500–508.


.webp)