Importance of MRD
The Deepest Level of Treatment Response in Multiple Myeloma
Deeper treatment responses drive improved outcomes1-3
MRD describes the low level of malignant cells that persist in the bone marrow after treatment but cannot be detected with conventional outcome measures and which eventually lead to relapse. A patient who is MRD negative has achieved clinical remission with the absence of aberrant clonal cells by NGF or NGS per at least 100,000 nucleated cells.3,4
Numerous studies suggest that MRD negativity may surpass CR as a prognostic marker for PFS and OS. Results demonstrating the prognostic superiority of MRD negativity have been seen across treatment regimens and regardless of patient characteristics, including cytogenetic risk, in NDMM and RRMM.1,5
MRD- is associated with improved rates of survival in NDMM and RRMM1
In a large meta-analysis evaluating patients with NDMM and RRMM, patients achieving MRD- experienced significantly longer OS and PFS vs MRD+ patients1
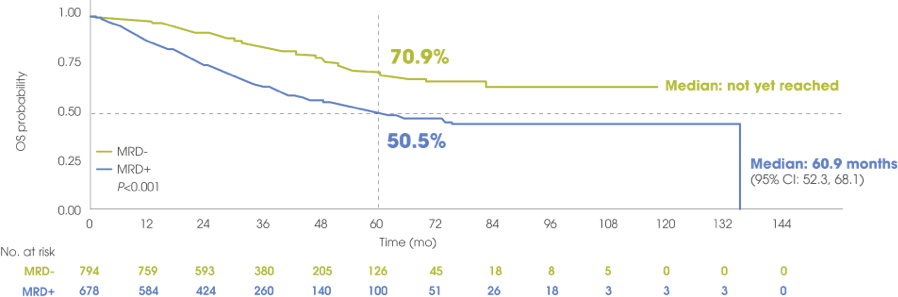
OS by MRD status in NDMM
Transplant-eligible NDMM: MRD- is associated with prolonged OS vs MRD+
Adapted from Munshi NC et al. Blood Adv. 2020.
Five-year OS rates were 70.9% for MRD- patients vs 50.5% for MRD+ patients.
The same trend toward improved survival was observed among patients with transplant-ineligible NDMM (N=1268) where MRD- was also associated with significantly improved OS vs MRD+ (HR=0.40; 95% CI: 0.31, 0.51; P<0.001). In the meta-analysis, a pooled Kaplan-Meier curve for OS by MRD status was not generated because it was only reported in 1 study.
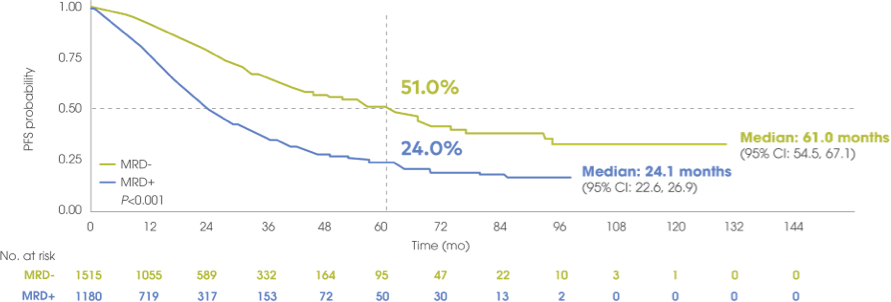
PFS by MRD status in NDMM
Transplant-eligible NDMM: MRD- is associated with prolonged PFS vs MRD+
Adapted from Munshi NC et al. Blood Adv. 2020.
Five-year PFS rates were 51% for MRD- patients vs 24% for MRD+ patients.
The same trend toward improved PFS was observed among patients with transplant-ineligible NDMM (N=2350) who achieved MRD- vs patients who were MRD+ (HR=0.32; 95% CI: 0.27, 0.39; P<0.001).
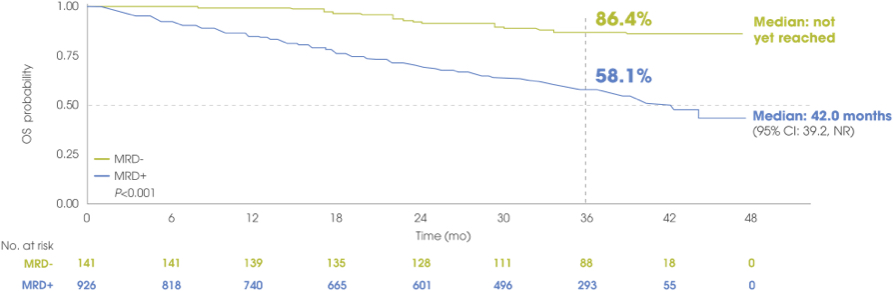
OS by MRD status in RRMM
RRMM: MRD- is associated with prolonged OS vs MRD+
Adapted from Munshi NC et al. Blood Adv. 2020.
Three-year OS rates were 86.4% for MRD- patients vs 58.1% for MRD+ patients.
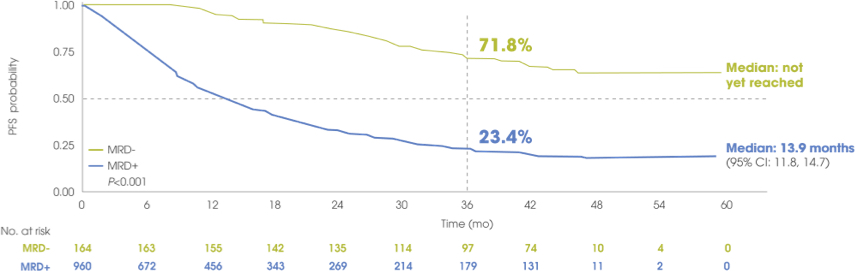
PFS by MRD status in RRMM
RRMM: MRD- is associated with prolonged PFS vs MRD+
Adapted from Munshi NC et al. Blood Adv. 2020.
Three-year PFS rates were 71.8% for MRD- patients vs 23.4% for MRD+ patients.
MRD- may surpass CR as the most powerful indicator of long-term outcomes1,5,6
With treatment advances in MM leading to an increasing proportion of patients achieving CR, particularly in first-line therapy, the development of MRD testing has given investigators a tool to detect even deeper treatment responses for a more accurate prognostic assessment.1,2
As superior outcomes have been observed in patients achieving MRD- compared to patients achieving CR with persistent residual disease, MRD- may supersede the prognostic value of CR.1,5,6
A pooled analysis of patients with NDMM who achieved CR but remained MRD+ showed a greater risk of relapse and disease progression vs patients who achieved CR and MRD-5
- Patients in CR with persistent MRD (MRD+) = 27 months
- Patients in CR with undetectable MRD (MRD-) = 63 months
Compared to achieving CR alone, achieving MRD negativity can significantly prolong disease control and delay relapse1,5,6
Achieving MRD- can overcome the poor prognosis of high-risk cytogenetics7
Although patients with both standard and high-risk cytogenetics achieve similar CR rates, the latter typically experience significantly earlier relapse.
However, a recent study of patients with transplant-eligible NDMM showed that treatment leading to MRD- overcame the poor prognosis conferred by high-risk cytogenetics, with 3-year PFS rates >90% for patients achieving MRD-, regardless of cytogenetic risk status.
Rate of PFS at 36 months by cytogenetic risk and MRD status7
Patients with high-risk cytogenetics who achieve MRD negativity may have outcomes that are comparable to standard risk patients, depending on MRD status7
Looking to treatments that achieve high rates of MRD negativity for patients is increasingly important to ensure better outcomes4,8
CR=complete response; MM=multiple myeloma; mPFS=median progression-free survival; MRD=minimal residual disease; MRD-=minimal residual disease negativity; MRD+=minimal residual disease positivity; NDMM=newly diagnosed multiple myeloma; NGF=next-generation flow; NGS=next-generation sequencing; OS=overall survival; PFS=progression-free survival; PR=partial response; RRMM=relapsed and/or refractory multiple myeloma; sCR=stringent complete response; VGPR=very good partial response.
- Munshi NC, Avet-Loiseau H, Anderson KC, et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 2020;4(23):5988-5999.
- Burgos L, Puig N, Cedena M-T, et al. Measurable residual disease in multiple myeloma: ready for clinical practice? J Hematol Oncol. 2020;13(1):82.
- Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328-e346.
- Kostopoulos IV, Ntanasis-Stathopoulos I, Gavriatopoulou M, Tsitsilonis OE, Terpos E. Minimal residual disease in multiple myeloma: current landscape and future applications with immunotherapeutic approaches. Front Oncol. 2020;10:860.
- Lahuerta J-J, Paiva B, Vidriales M-B, et al. Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J Clin Oncol. 2017;35(25):2900-2910.
- Martinez-Lopez J, Wong SW, Shah N, et al. Clinical value of measurable residual disease testing for assessing depth, duration, and direction of response in multiple myeloma. Blood Adv. 2020;4(14):3295-3301.
- Goicoechea I, Puig N, Cedena M-T, et al. Deep MRD profiling defines outcome and unveils different modes of treatment resistance in standard- and high-risk myeloma. Blood. 2021;137(1):49-60.
- Landgren O, Iskander K. Modern multiple myeloma therapy: deep, sustained treatment response and good clinical outcomes. J Intern Med. 2017;281(4):365-382.