The Lixilan-L Study

Efficacy and safety of LixiLan, a Titratable fixed-ratio combination of Insulin glargine plus Lixisenatide in Type 2 Diabetes inadequately controlled on Basal insulin and Metformin: The LixiLan-L randomized trial
Objective
Demonstrating the efficacy and safety of LixiLan (iGlarLixi), a novel, titratable, fixed-ratio combination of insulin glargine (iGlar) (100 units) and lixisenatide, compared with iGlar in patients with Type 2 diabetes inadequately controlled on Basal insulin with or without up to two oral glucose-lowering agents.¹
Study design
After a 6-week run-in# when iGlar was introduced and/or further titrated, and oral antidiabetic drugs other than metformin were stopped, HbA1c decreased from 8.5% to 8.1% then a total of 736 basal insulin-treated patients were randomized 1:1 for 30 weeks to:1

both titrated to fasting plasma glucose <100 mg/dL (<5.6 mmol/mol) up to a maximum dose of 60 units/day.
# Eligible patients entered a 6-week run-in phase during which any OAD other than metformin was stopped, patients were switched to iGlar (if they had previously been receiving another basal insulin), and the daily dose of iGlar was titrated and/or stabilized for all patients.
Endpoints¹
Primary efficacy endpoint: Change in HbA1c from baseline to week 30
Secondary efficacy endpoint:
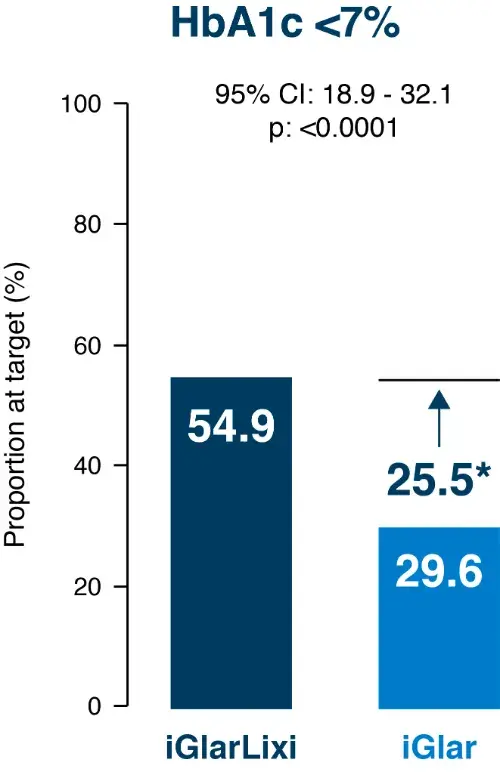
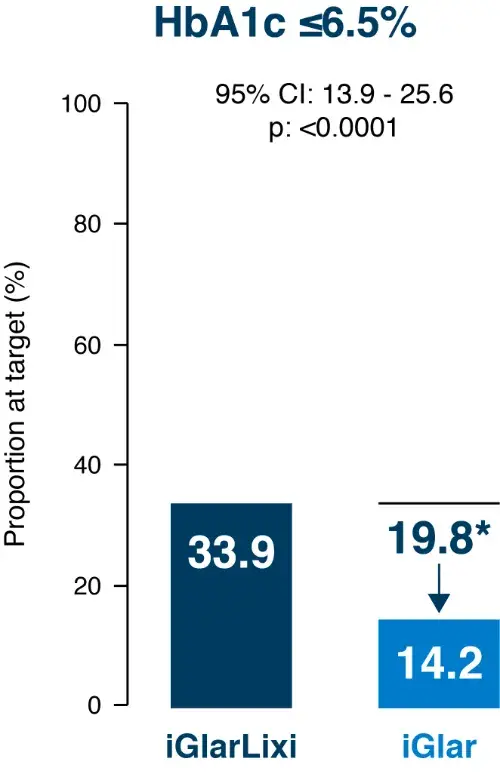
- The percentage of patients reaching target HbA1c <7.0% (53 mmol/mol) and ≤6.5% (48 mmol/mol) at week 30
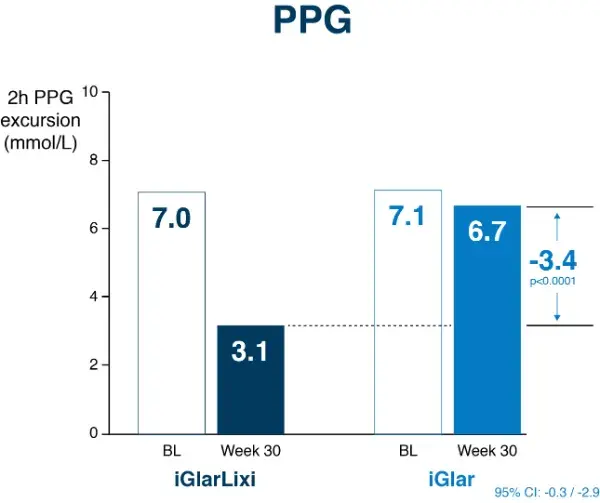
- Change in 2-h PPG during the standardized liquid meal test.
- Change in bodyweight
- Change in average 7-point SMPG profile
- Percentage of patients reaching HbA1c <7% (53 mmol/mol) with no body weight gain at week 30
- Percentage of patients reaching HbA1c <7% (53 mmol/mol) with no body weight gain at week 30 and no documented symptomatic hypoglycemia during treatment
- iGlar daily dose
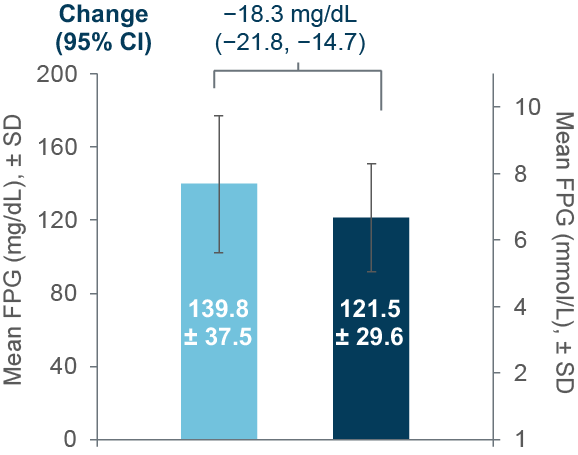
- FPG
- Percentage of patients reaching HbA1c <7% (53 mmol/mol) at week 30 with no documented symptomatic hypoglycemia (PG ≤70 mg/dL [3.9 mmol/L]) during the 30-week randomized treatment period
- Percentage of patients requiring rescue therapy during the 30-week randomized treatment period.
Safety endpoint: Symptomatic hypoglycemia and gastrointestinal adverse events
Results
Primary efficacy endpoint

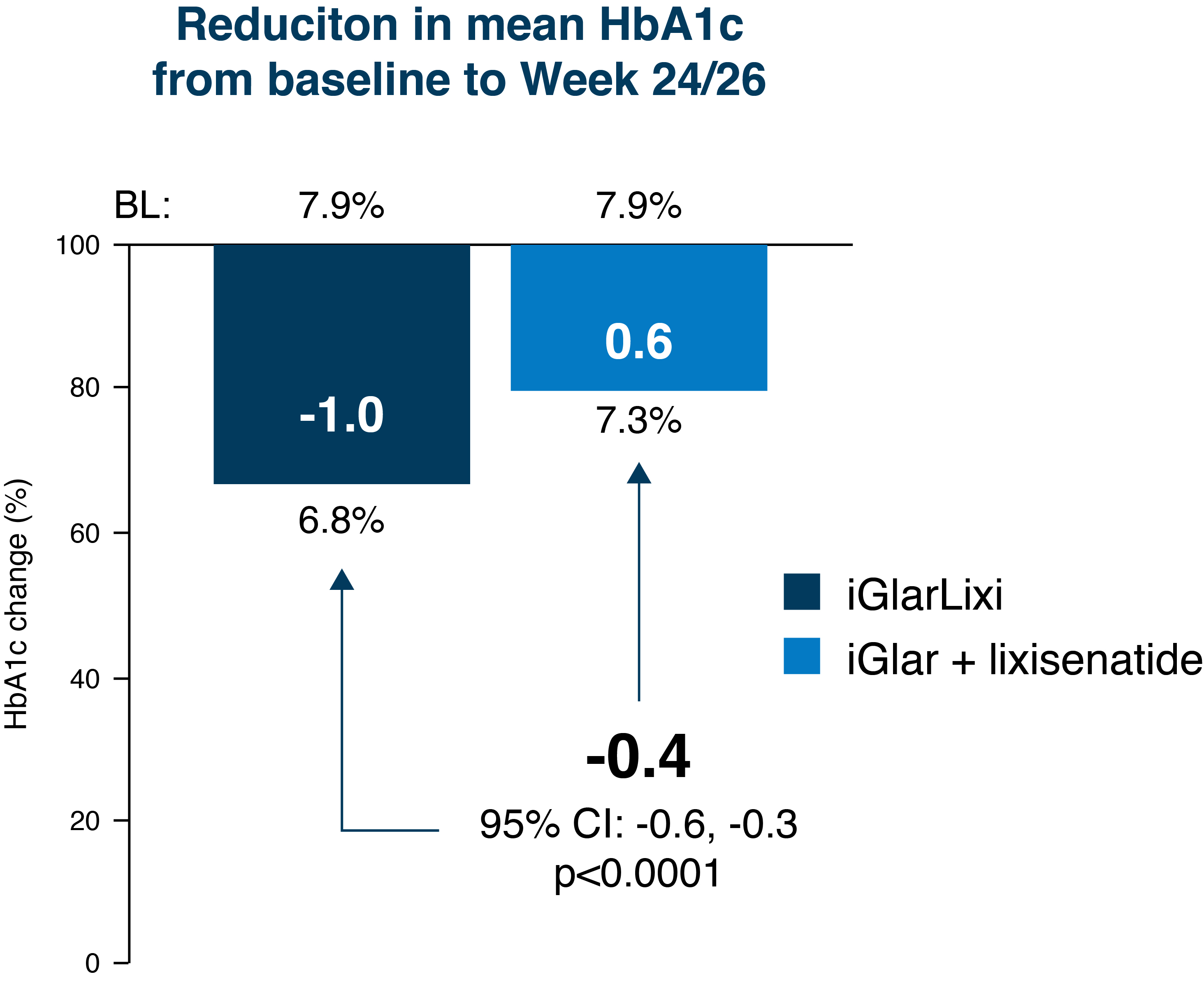
- Statistical superiority of iGlarLixi over iGlar was demonstrated for the change in HbA1c from baseline to week 30 (LS mean difference vs. iGlar –0.5%; 95% CI –0.6, –0.4; P<0.0001)1
- Mean HbA1c levels were reduced more with iGlarLixi than with iGlar (-1.1% vs. – 0.6%, respectively), achieving final HbA1c levels of 6.9% (52 mmol/mol) for iGlarLixi and 7.5% (58 mmol/mol) for iGlar after 30 weeks of treatment.1
Secondary efficacy endpoint
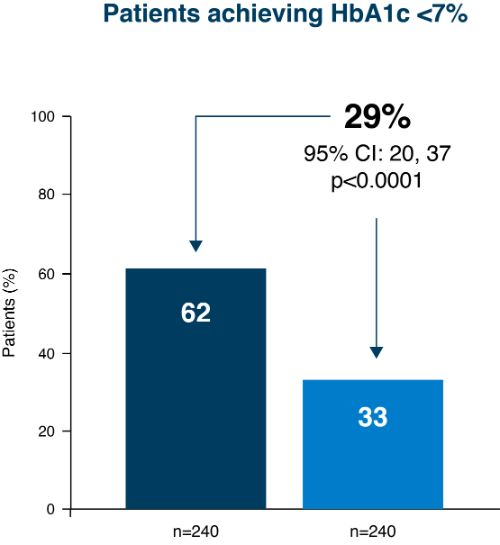
- People achieving HbA1c target at week 30 Significantly greater proportion reached target with iGlarLixi vs. iGlar1
- Effect of iGlarLixi on FPG and PPG iGlarLixi combines the FPG effect of iGlar and the PPG effect of Lixi1,2
.webp)
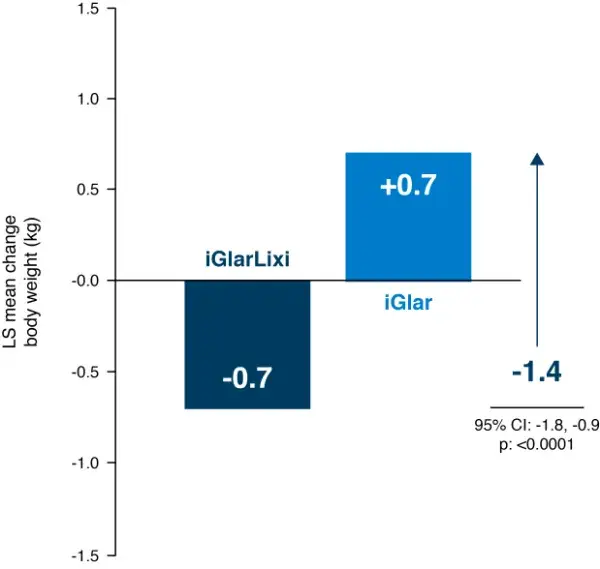
- Changes in body weight iGlarLixi was not associated with the weight gain often seen with insulin therapy¹
Safety endpoint
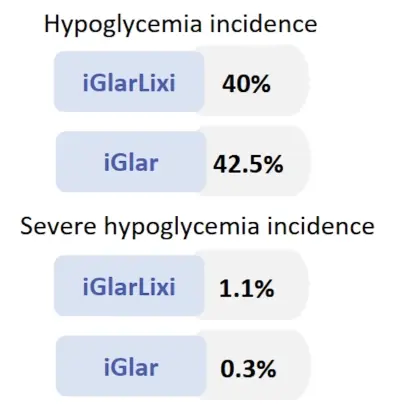
- Similar hypoglycemia with iGlarLixi vs. iGlar despite significantly better HbA1C with iGlarLixi1
Summary¹
- The primary objectives of the study were met as superiority of iGlarLixi in HbA1c change from baseline was shown versus iGlar.
- During the run-in, HbA1c was reduced from 8.5% to 8.1%
- Subsequent introduction of iGlarLixi (+ continuation of metformin where applicable):
- Further improved HbA1c from 8.1% to 6.9%
- Reduced 2 hour-PPG and glucose excursions was associated with weight reduction (-0.7 kg) with a significant difference of 1.4 kg versus iGlar (p<0.0001)
- 55% of people achieved HbA1c <7%
- 34% with HbA1c <7% and no weight gain
- 32% with HbA1c <7% and no documented hypoglycemia
- The incidence of documented symptomatic hypoglycemia (≤70 mg/dL) was similar in the iGlarLixi and iGlar treatment groups
- Overall, iGlarLixi was well tolerated with a safety profile reflecting those of iGlar and lixisenatide
Post-Hoc analysis of Lixilan-L study³
At each baseline HbA1c level, more people reached HbA1c <7.0% with iGlarLixi
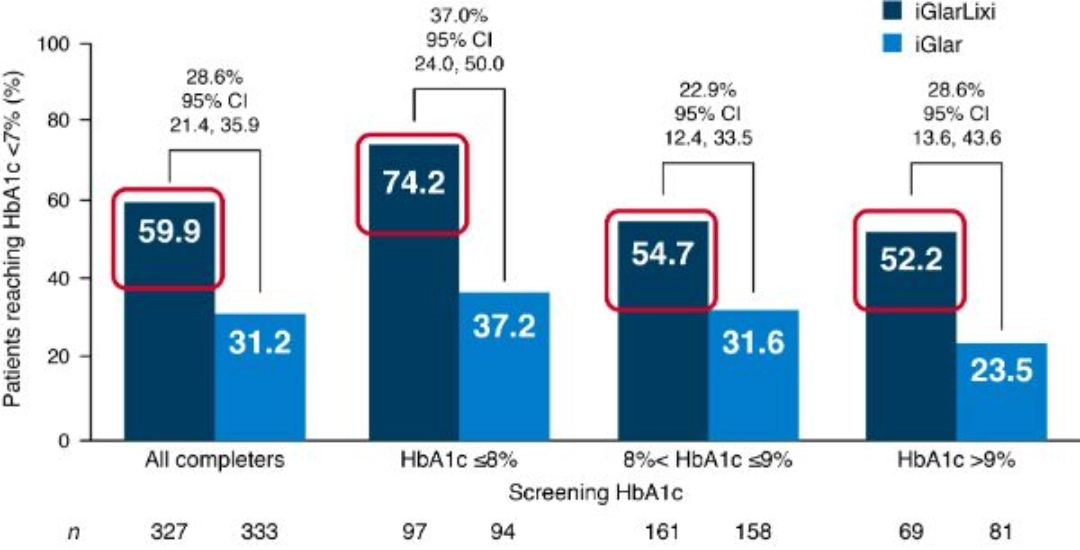
This post hoc analysis of the LixiLan-L trial included both the screening phase and the treatment period for 30-week completers and evaluated the change in HbA1c from screening to Week 30, patients reaching HbA1c<7% at Week 30, and iGlar and lixisenatide (Lixi) doses at Week 30 overall and according to HbA1c subcategoryat screening (HbA1c ≤ 8%, 8%<HbA1c ≤9 %, and HbA1c> 9%)
Indirect comparison: iGlarLixi in Lixilan-L and sequential iGlar + lixisenatide in GetGoal Duo-2⁴
iGlarLixi was associated with greater HbA1c reductions than sequential intensification with insulin glargine + lixisenatide
iGlarLixi showed numerically greater improvements in FPG and PPG compared with sequential intensification
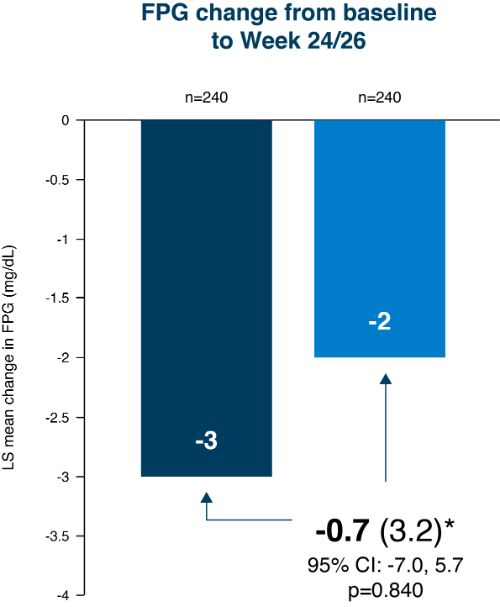
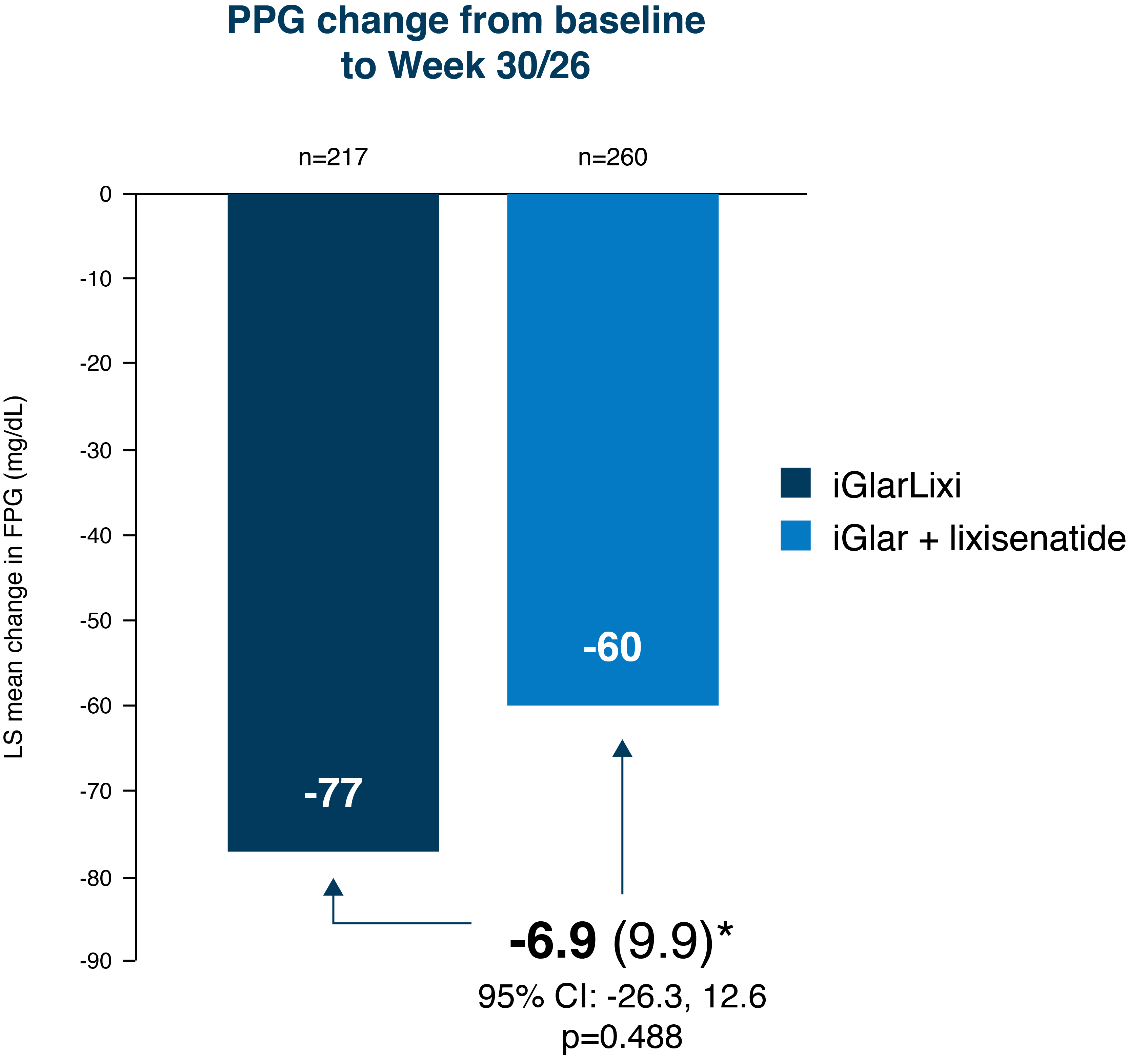
*LS mean difference (standard error). Modified intent-to-treat population
Dosing⁵
1. iGlarLixi dosing in patients with previous basal insulin dose* ≥20, <30 U
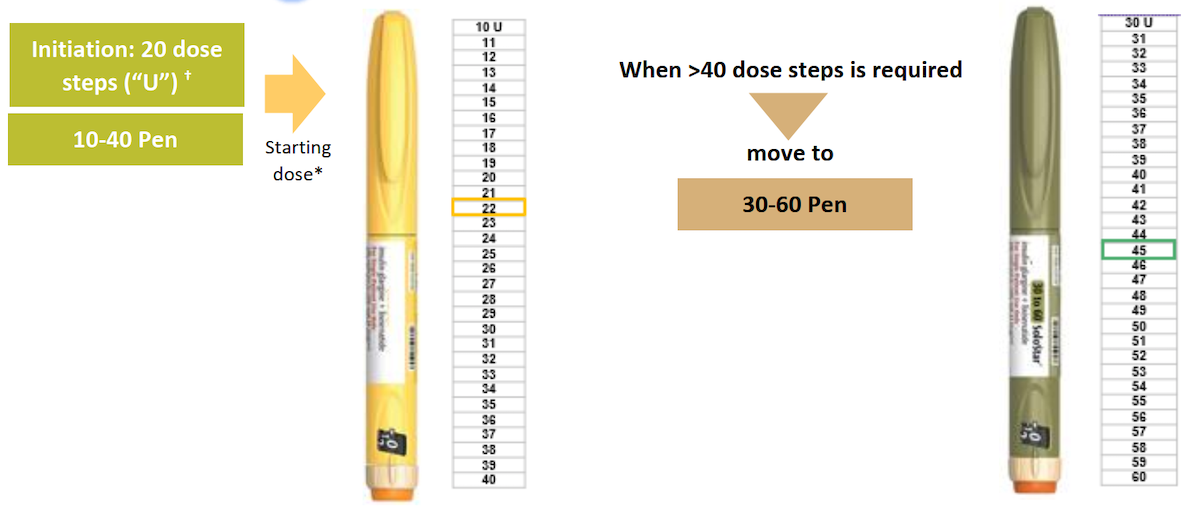
2. iGlarLixi dosing in patients with previous basal insulin dose ≥30, ≤60 U
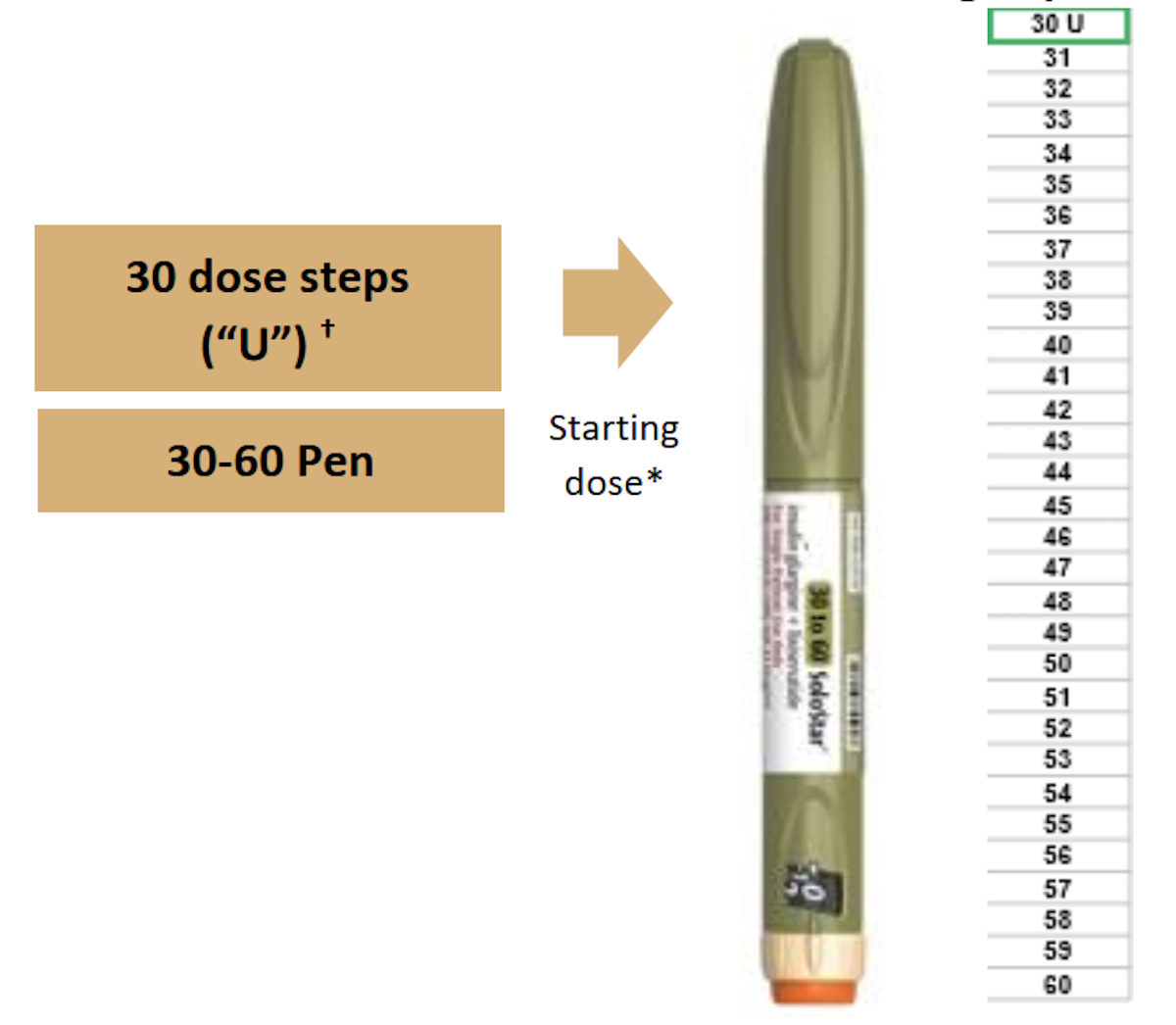
*Therapy with basal insulin or GLP-1 RA or OAD other than metformin and SGLT2 inhibitors should be discontinued prior to initiation of Suliqua. Starting doses are based on previous insulin glargine 100 U/mL dose. For twice daily basal insulin or insulin glargine (300 units/ml), the total daily dose previously used should be reduced by 20% to choose the Suliqua starting dose. For any other basal insulin the same rule as for insulin glargine (100 units/ml) should be applied.
†Each dose step contains 1 unit of insulin glargine and 0.33 micrograms of lixisenatide. The maximum daily dose is 60 units insulin glargine and 20 mcg lixisenatide corresponding to 60 dose steps. Consult prescribing information in your country as information and availability of the pens shown on the slide may vary.
iGlarLixi, insulin glargine and lixisenatide; iGlar, insulin glargine; PPG, postprandial plasma glucose; FPG, fasting plasma glucose; GLP-1 RA, glucagon-like peptide-1 receptor agonist; OAD, oral antihyperglycemic drug; SMPG, self-monitored plasma glucose; SU, sulfonylureas; SGLT-2, Sodium/glucose cotransporter 2
- Aroda, V., Rosenstock, J., Wysham, C., Unger, J., Bellido, D., González-Gálvez, G., Takami, A., Guo, H., Niemoeller, E., Souhami, E. and Bergenstal, R., 2016. Efficacy and Safety of LixiLan, a Titratable Fixed-Ratio Combination of Insulin Glargine Plus Lixisenatide in Type 2 Diabetes Inadequately Controlled on Basal Insulin and Metformin: The LixiLan-L Randomized Trial. Diabetes Care, 39(11), pp.1972-1980.
- Fda.gov. 2016. Lixisenatide and iGlarLixi Type 2 Diabetes Mellitus. [online] Available at: <https://www.fda.gov/media/98525/download> [Accessed 27 May 2021].
- Niemoeller, E., Souhami, E., Wu, Y. and Jensen, K., 2018. iGlarLixi Reduces Glycated Hemoglobin to a Greater Extent Than Basal Insulin Regardless of Levels at Screening: Post Hoc Analysis of LixiLan-L. Diabetes Therapy, 9(1), pp.373-382.
- Meier JJ, et al. Presented at ADA 2017, San Diego (CA), US: Abstract 2386
- Adapted from: Rosenstock, J., Cheng, A., Ritzel, R., Bosnyak, Z., Devisme, C., Cali, A., Sieber, J., Stella, P., Wang, X., Frías, J., Roussel, R. and Bolli, G., 2018. More Similarities Than Differences Testing Insulin Glargine 300 Units/mL Versus Insulin Degludec 100 Units/mL in Insulin-Naive Type 2 Diabetes: The Randomized Head-to-Head BRIGHT Trial. Diabetes Care, 41(10), pp.2147-2154. Highlights from the EU SmPC are provided here; please refer to the SmPC for more detailed information. Available at: https://www.ema.europa.eu/en/documents/product-information/suliqua-eparproduct-information_en.pdf (Last accessed December 2019)



