Event rates and Risk Factors for Recurrent CV Events
Key Takeaway
RWE study based on this large, representative, and well-characterised US population cohort that was followed after discharge from ACS hospitalization showed that:
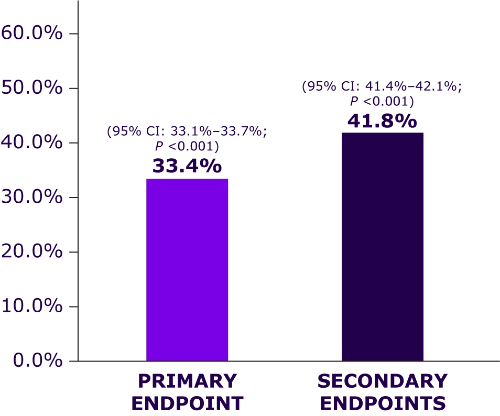
The 5-year event rate for the primary composite endpoint* was 33.4%
- Highest in subgroups such as MI without revascularization and Thrombolysis In Myocardial Infarction Risk Score for Secondary Prevention (TRS 2oP) ≥4
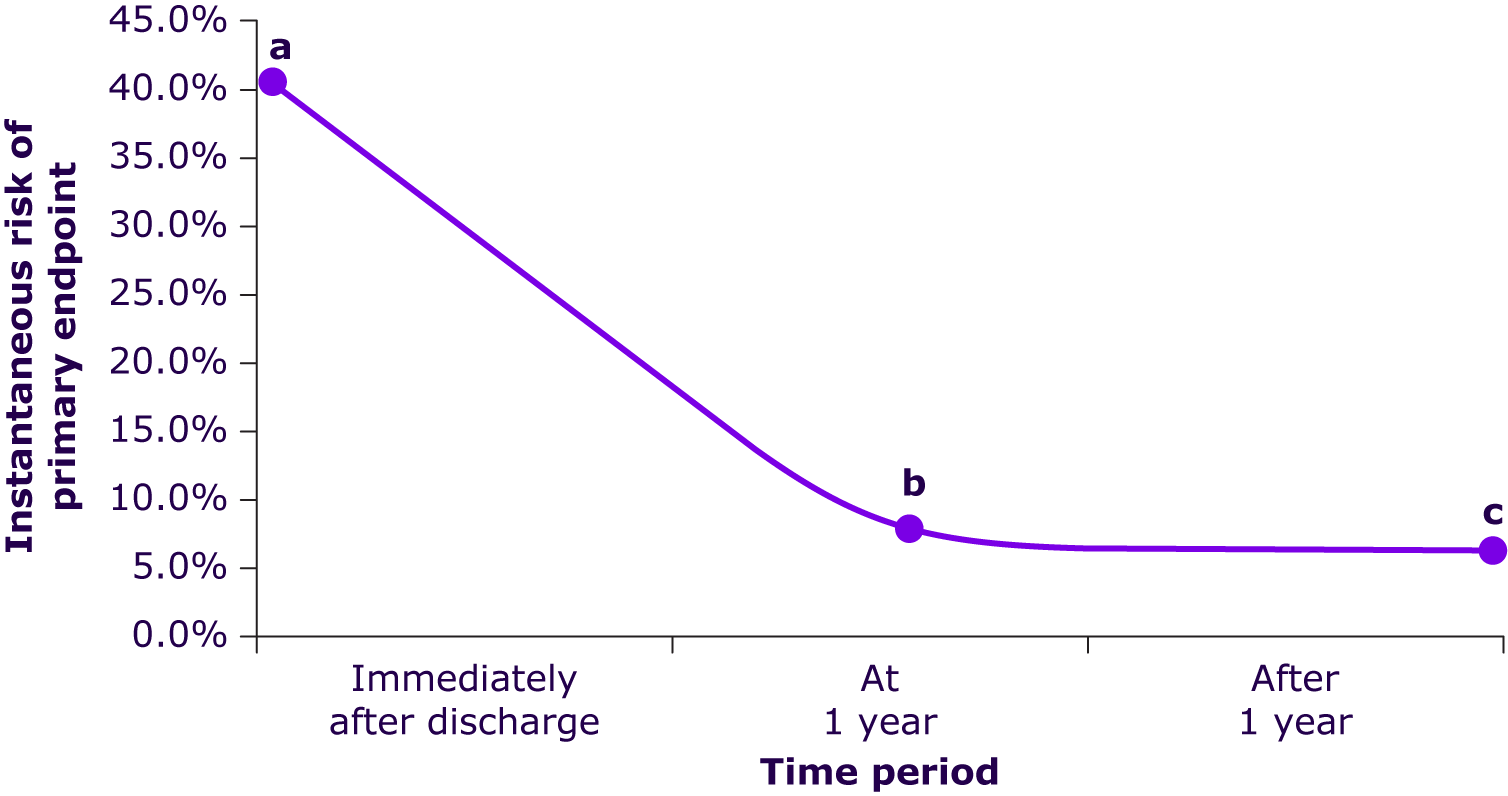
Patients with ACS remain at very high risk of experiencing recurrent CV events, particularly early after discharge
- Risk of experiencing the primary composite endpoint was ≈6-fold higher immediately after discharge vs ≥1 year after hospital discharge
These findings support the potential application of the TRS 2oP for informed decision-making (to multiple stakeholders including payers, regulatory authorities, clinicians and clinical guidelines committees) in clinical management of ACS, identification of patients at highest risk, and development of future guidelines.
Why This Matters
Guidelines identified that patients with ACS remain at higher risk for future adverse outcomes.
Evidence from contemporary, representative ACS populations in a clinical practice setting is needed for identifying subgroups and strategies that improve patient outcomes.
This study evaluated a large, representative, well-characterized cohort of patients hospitalized with ACS to better understand recurrent risk and risk predictors in a US clinical practice population.
Study Design
This study cohort included patients (N = 594,032) with evidence of an ACS hospitalization (index ACS) from the Optum Research Database between January 1, 2005, and December 30, 2018.
Additional inclusion criteria
- Age ≥20 years
- Availability of 1-year baseline data before the index date
- Discharge codes indicative of alive status
Exclusion criteria
- Patients with a history of heart transplantation
Subgroups
- Based on index ACS event (MI/UA), revascularization status, and the TRS 2oP
Endpoints assessed
- Primary composite endpoint: First occurrence of CV death, nonfatal MI, or nonfatal ischemic stroke
- Secondary endpoints: First occurrence of CV death, nonfatal MI, nonfatal ischemic stroke, nonfatal UA hospitalization, and nonfatal elective coronary revascularization, separately and as a composite
Key Results
Overall, 239,234 patients were included and were followed up for a median of 1.2 (IQR, 0.4–2.8) years.
|
Patient-characteristics |
• Mean age = 69.2 years |
|
5-year rates for the primary and secondary endpoints |
|
Highest rate of the primary endpoint in subgroups |
.webp)
|
Risk for primary endpoint (First occurrence of CV death, nonfatal MI, or nonfatal ischemic stroke) |
a. The instantaneous risk for the primary endpoint was (40.9%) immediately after discharge
b. It gradually to ≈6.7% at 1 year of follow-up
c. Risk remained gradually after 1 year (≈6.4%)
Risk Factors Most Strongly Associated† With the Primary Endpoint
Age ≥65 years

Heart failure

Renal disease stages IV–V

History of Ischemic stroke

An index MI without revascularization
ACS hospitalization in last 12 months
Limitations
- This analysis might not be representative of the noninsured population, those covered under a public insurance program other than Medicare Advantage, or international populations.
- Claims database captured medications that received only under health plan.
- Clinical trials typically classify patients into ST vs non-ST-segment-elevation MI by electrocardiographic review, which could not be reliably done using claims data.
- Several biomarkers that have shown to offer useful prognostication on top of clinical risk predictors (e.g., TRS 2oP) were not typically collected in a manner that enables their incorporation in this analysis.
- During the identification period (2005–2018), the US changed MI definitions based on biomarkers, which likely affected the classification of MI vs UA in clinical practice over this period.
- Randomized clinical trials used for comparing this study were global trials, whereas this study population represents only patients in the US.
*Nonfatal MI, nonfatal ischemic stroke, or cardiovascular death
†Hazard ratio, >1.5; P <0.001
ACC/AHA, American College of Cardiology/American Heart Association; ACS, Acute coronary syndrome; CI, confidence interval; CV, cardiovascular; IQR, interquartile range; MI, myocardial infarction; RWE, real-world evidence; TRS 2oP, Thrombolysis In Myocardial Infarction Risk Score for Secondary Prevention; UA, unstable angina; US, United States.
- Steen DL, Khan I, Andrade K, Koumas A, Giugliano RP. Event rates and risk factors for recurrent cardiovascular events and mortality in a contemporary post acute coronary syndrome population representing 239 234 patients during 2005 to 2018 in the United States. J Am Heart Assoc. 2022;11(9):e022198. doi: 10.1161/JAHA.121.022198. PMID: 35475346.


.webp/jcr:content/jcr_content%20(9).webp)