Major GI Bleeding in VTE RIETE Analysis
Major gastrointestinal bleeding in patients with venous thromboembolism receiving anticoagulant therapy:
Results from Riete registry.
Key Takeaway
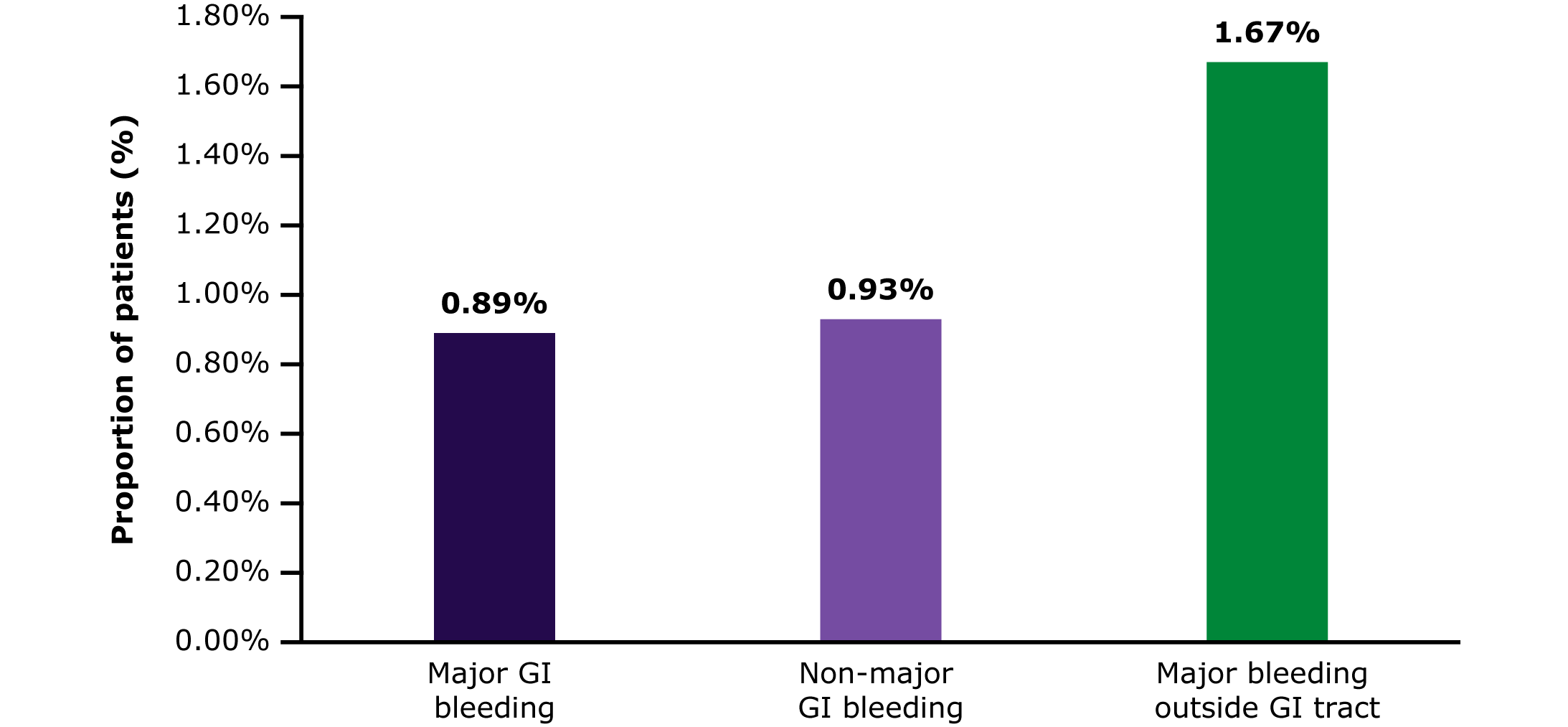
Analysis of clinical characteristics of patients with acute DVT/PE from RIETE* prospective registry database, who developed major GI bleeding during anticoagulant therapy showed that:
-
One in every 112 patients (0.89%) suffered major GI bleeding
-
One in every 107 patients (0.93%) had non-major GI bleeding
-
One in every 60 patients (1.67%) had major bleeding outside GI tract
- One in every 3 patients who suffered major bleeding died within the first 30 days
-
Variables independently predicting the risk for major GI bleeding:
-
Male sex, age ≥70 years, initial presentation as PE (vs isolated DVT), active cancer, prior VTE, recent major bleeding in the GI tract, esophageal varicosities, anemia, abnormal prothrombin time, renal insufficiency and concomitant therapy with corticosteroids
-
-
Predictive score developed focusing on GI bleeding showed that:
-
45% had low risk (major GI bleeding rate = 0.21%)
-
42% had intermediate risk (major GI bleeding rate = 0.96%)
-
11% had high risk (major GI bleeding rate = 2.41%)
-
2.2% had very high risk (major GI bleeding rate = 6.08%)
-
-
Predictive score has the potential to identify patients at increased risk for GI bleeding, who might theoretically benefit from use of safer anticoagulant drugs, avoidance of unnecessary corticosteroids, close monitoring of early signs of bleeding, or use of PPI
Why This Matters
Major GI bleeding is an early severe complication in patients receiving anticoagulant therapy for VTE.
- Early identification of at risk patients may help to better individualize VTE management to decrease the risk of GI bleeding
A predictive score based on multivariable analysis was developed to reliably identify patients at increased risk for major and fatal GI bleeding at the baseline.
Study Design
Data was obtained from the RIETE registry (NCT02832245).
- Patients included: Consecutive patients with acute, symptomatic VTE† and those with isolated distal DVT at baseline/ with isolated sub-segmental PE
- Comparison of clinical characteristics: Patients developing major GI bleeding during anticoagulant therapy vs non-major GI bleeding, major bleeding outside the GI tract and no bleeding
- Multivariable analysis: Identified independent predictors for major bleeding in the GI tract
- Predictive score: Built by assigning points to each independent variable according to regression coefficients ß
Key Results
A total of 87,431 patients were included in the analysis from March 2001 to March 2021.
Patients with GI/Non-GI bleeding during Anticoagulation
(median [IQR] days: 182 [101–315])
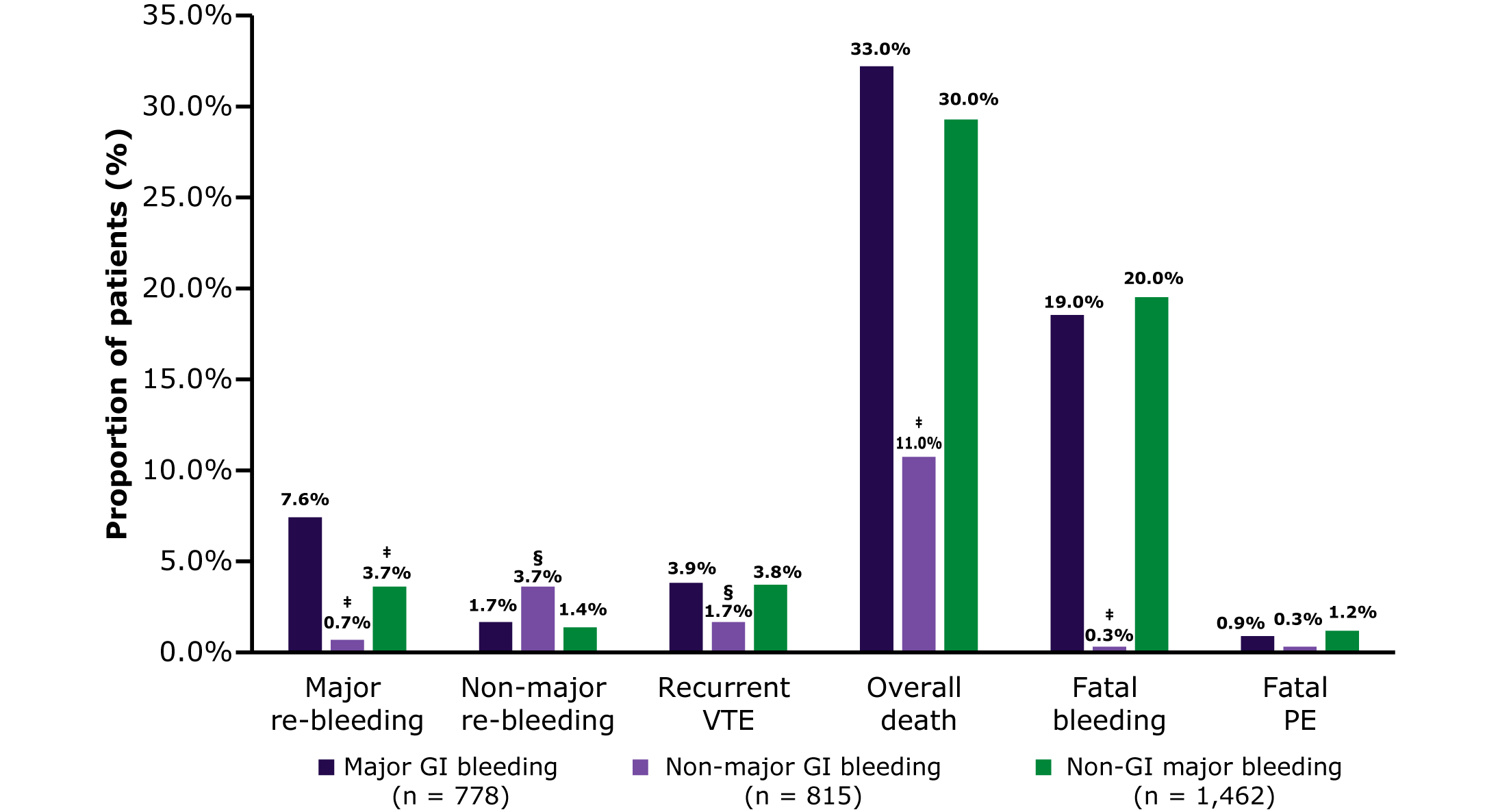
Outcomes reported during the first 30 days of therapy
For details about cumulative incidence of bleeding complications during first 365 days, click on the hyperlink.
Comparison of clinical characteristics
-
Patients with bleeding complications vs no bleeding were:
-
Older
-
Weighed less
-
More likely to initially present as symptomatic PE vs DVT alone
-
Had recent immobility or active cancer
-
Less likely to use hormonal therapy/be pregnant
-
-
Patients with bleeding complications vs no bleeding were more likely to have:
-
Anemia
-
Thrombocytopenia
-
Abnormal prothrombin time
-
Renal insufficiency at baseline
-
Antiplatelet/corticosteroid use
-
-
Patients with major bleeding in the GI tract vs patients with non-major GI bleeding/ major non-GI bleeding/no bleeding were more likely to have:
-
Cancer
-
Recent (<30 days before) major GI bleeding at baseline
-
Non-cancer lesions in the GI tract¶
-
For details about the results of multivariable analysis, click on the hyperlink.
Risk assessment by prognostic score
| Patient cohort | Major GI bleeding | Fatal GI bleeding | Non-major GI bleeding | Major non-GI bleeding |
|
Low risk (n = 39,591) |
0.21% | 0.002% | 0.52% | 0.79% |
|
Intermediate risk (n = 36,602) |
0.96% | 0.15% | 1.06% | 2.23% |
|
High risk (n = 9,315) |
2.41% | 0.63% | 1.78% | 3.16% |
|
Very high risk (n = 1,923) |
6.08% | 1.66% | 2.81% | 2.08% |
|
c-statistics |
0.771 | 0.864 | 0.656 | 0.657 |
|
95% CI |
0.755-0.786 | 0.841-0.886 | 0.637-0.674 | 0.645-0.669 |
Limitations
- This was a post-hoc analysis of prospectively collected data in unselected patients with acute VTE.
- Analysis was not a-priori calibrated to assess the hypothesis and may be underpowered
- Management of patients for acute VTE and bleeding was left to investigators and local usual care
- Differences pertaining to initial choice of anticoagulant therapy may have been guided by the clinical perception of bleeding risk
- Score was not externally validated using another cohort of patients
For additional details, please refer to the source publication Catella J, et al.
*The RIETE database is an ongoing, multicenter, international, prospective registry
†Confirmed by objective tests (ventilation-perfusion lung scan, helical CT-scan or contrast angiography for patients with clinically suspected PE; compression ultrasonography or contrast venography for those with suspected DVT
‡P <0.001
§P <0.05
¶Such as hiatal hernia, gastroduodenal ulcer, cirrhosis, esophagitis, esophageal varicosities or angiodysplasia
Abbreviations
CI, confidence interval; DVT, deep vein thrombosis; GI, gastrointestinal; IQR, interquartile range; PE, pulmonary embolism; PPI, proton pump inhibitors; RIETE, Registro Informatizado Enfermedad TromboEmbÓlica; SD, standard deviation; VTE, venous thromboembolism.
- Catella J, Bertoletti L, Moustafa F, Nieto JA, Valle R, Pedrajas JM, et al. Major gastrointestinal bleeding in patients receiving anticoagulant therapy for venous thromboembolism. Thromb Res. 2022;214:29–36. doi: 10.1016/j.thromres.2022.04.005. PMID:35452869

.jpg0/jcr:content/science%20hero%20(3).jpg)
.png)
.png)