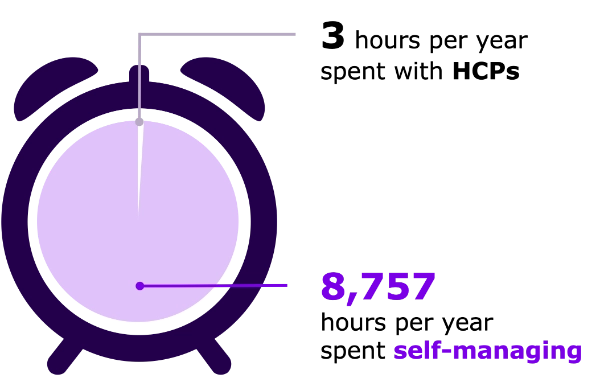
The burden associated with insulin self-management
The burden associated with insulin self-management is high and People With Diabetes are responsible for most of their daily regimen
HCP, healthcare professional; PWD, person with diabetes. Diabetes UK. Diabetes Education and Self-Management. Available at:
https://www.diabetes.org.uk/professionals/resources/shared-practice/diabetes-education#:~:text=Use%20the%20following%20resources%20and,year%20with%20a%20healthcare%20professional (last accessed September 2023)
With this high burden on the individual with diabetes, concordance to insulin therapies remains low
People with T2D may be likely to miss, mistime or reduce their basal insulin doses
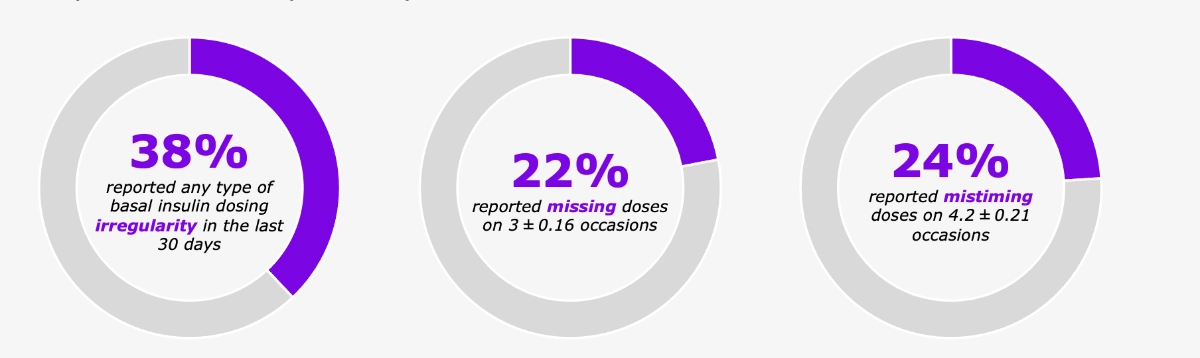
A large proportion of missed or mistimed basal insulin doses were reported as unintentional,
whereas the majority of reduced basal insulin doses were reported as intentional
The GAPP2 study was an online multinational cross-sectional study of people with T2D currently treated with basal insulin (N=3,042), and HCPs involved in the care of such people. Basal insulin concordance patterns were evaluated with respect to three types of dosing irregularity: missed, mistimed [±2 hours from prescribed time], and reduced dose over the last 30 days. A total of 3,042 people with T2D treated with basal insulin analogs and 1,222 prescribers completed the full survey. GAPP2, Global Attitude of Patients and Physicians 2. Brod M, et al. Curr Res Med Opin 2012;28:1933–46.
Multiple barriers exist to facilitate and maximize concordance to basal insulin therapy
![]()

Psychological burden on people
with diabetes

Time burden regarding dosing
and recording
Struggle with injections (missed doses)
![]()
Little understanding of impact of insulin and
lifestyle on glycemic variability

Physicians do not know the extent of glycemic
variability’s impact on a person’s daily life
![]()

Feelings of guilt and embarrassment, and
perception as a burden on the system

Lack of data sharing with healthcare provider
owing to fears of judgement

Time spent during consultation is generally low
Peyrot, M, et al. Diabet Med 2012;29:682–9; Berard L, et al. Diabetes Obes Metab 2018;20:301–8; Ampudia–Blasco FJ, et al. Endocrinología y Nutrición 2014;61:426–33.