The Future of MRD

It May Be Time for a New Standard for Measuring Depth of Response in Multiple Myeloma
Deeper response assessments are needed to keep pace with therapeutic advancements1-3
Although the assessment of MRD is not universally employed in clinical practice, numerous studies have demonstrated the considerable strength of MRD- as a reliable predictor of long-term outcomes, including the potential to supersede the prognostic value of CR.
MRD negativity continues to be investigated as a surrogate endpoint for survival in clinical trials and evaluated as a tool in clinical practice for informing individualised treatment decisions1,2
The evaluation of MRD in clinical trials may help accelerate regulatory approvals—especially in NDMM2,3,7
Given that recent therapeutic advances have significantly extended survival in multiple myeloma, a new surrogate endpoint is needed that predicts clinical benefit and accelerates drug development and approvals.2,3,5
Ongoing and future clinical trials in NDMM using the traditional primary endpoint of PFS may require ≥ 5 years to collect mature data, potentially delaying access to increasingly efficacious treatments.3
While there is not yet consensus among regulatory agencies, there are ongoing efforts to gather the necessary evidence to more clearly elucidate the role of MRD in clinical trials, clinical practice, and new drug registration.8
In NDMM and RRMM at least 35 ongoing phase 3 clinical trials include MRD assessment as a primary or second endpoint8
‘MRD has been found to be a surrogate endpoint for PFS in patients receiving first-line treatment. Therefore, MRD may be used as an endpoint to accelerate drug development.’
MA Dimopolous et al, Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up, Ann Oncol, 2021
Achieving MRD- should be considered a goal in first-line therapy6
The development of increasingly sensitive techniques for assessing treatment response have begun to challenge the conventional therapeutic goals of achieving CR or even sCR alone, particularly in NDMM.4-6
Treating to the deepest molecular response with MRD- as the ultimate goal represents a strategy of maximising outcomes for as many patients as possible4,6
mPFS 7.2 years seen in patients with NDMM when treating to achieve MRD negativity6
- Results from a retrospective analysis of real-world outcomes from a single US academic center (2005-2018), with patients primarily receiving triplet regimens followed by ASCT and maintenance therapy6
- Patients with NDMM (N=159) treated to achieve the deepest response per IMWG criteria saw considerably longer mPFS (86.4 months) than prior reports in similar settings (≤50 months)6,9,10
- Of 159 patients with NDMM, 98% achieved CR prior to MRD assessment and 59% achieved MRD- at 10-5 6
Evaluating therapies by demonstrated rate of MRD negativity may be crucial for maximising outcomes early for as many patients as possible6
In the future, MRD- may be used to guide therapeutic decisions11,12
Although evaluation of MRD is not yet a widespread factor in routine clinical decision-making, due in part to limited access to testing and still unresolved questions about the best use of MRD status in clinical practice, there is evidence to support further investigation of its role in treatment decisions.11
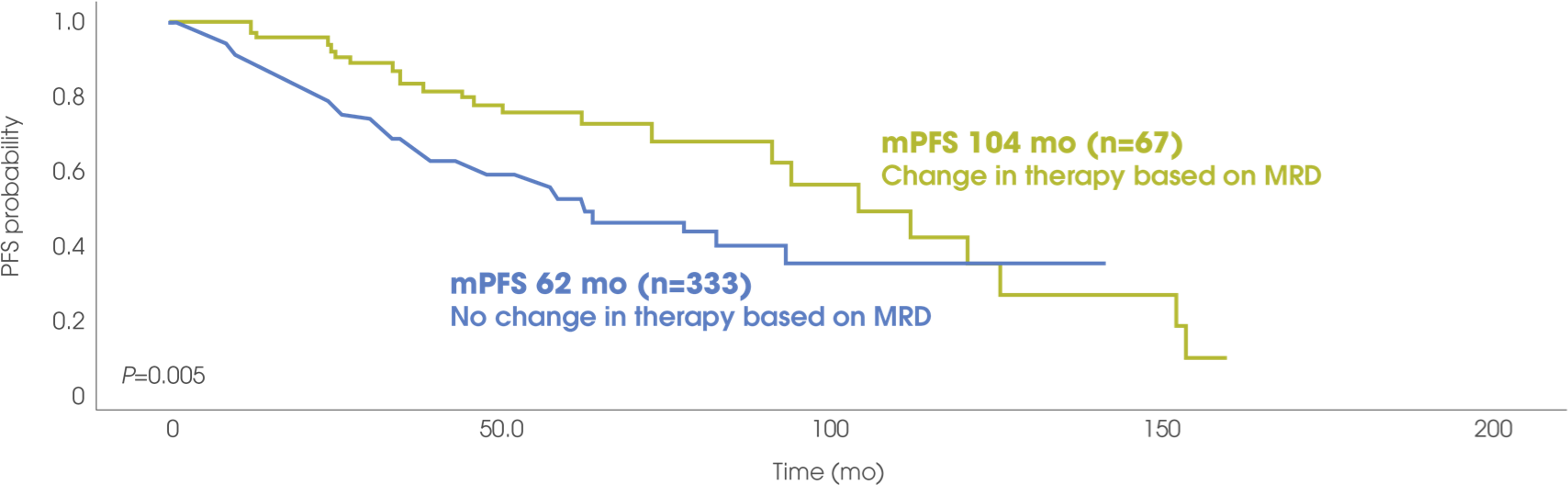
In a retrospective analysis of PFS in patients with NDMM, a clinical decision to change therapy was made in 17% of patients based on their MRD status (MRD- or MRD+ at 10-5).12
Patients for whom a change in therapy was made based on MRD status had prolonged PFS compared to those for whom a change in therapy was not made.12
Retrospective analysis of 400 patients with NDMM12
As MRD negativity continues to be investigated as a surrogate endpoint for PFS in NDMM clinical trials, there is clear and mounting evidence that MRD negativity is emerging as one of the most important clinical tools in the treatment of MM1,2,4-6
The assessment of MRD negativity is needed in the clinical setting to improve prognosis, maximise outcomes, and inform treatment decision-making1,7
ASCT=autologous stem cell transplant; CR=complete response; IMWG=International Myeloma Working Group; MM=multiple myeloma; mPFS=median progression-free survival; MRD=minimal residual disease; MRD-=minimal residual disease negativity; MRD+= minimal residual disease positivity; NDMM=newly diagnosed multiple myeloma; PFS=progression-free survival; RRMM=relapsed and/or refractory multiple myeloma; sCR=stringent complete response.
- Kostopoulos IV, Ntanasis-Stathopoulos I, Gavriatopoulou M, Tsitsilonis OE, Terpos E. Minimal residual disease in multiple myeloma: current landscape and future applications with immunotherapeutic approaches. Front Oncol. 2020;10:860.
- Dimopoulos MA, Moreau P, Terpos E, et al. Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32(3):309-322.
- Avet-Loiseau H, Ludwig H, Landgren O, et al. Minimal residual disease status as a surrogate endpoint for progression-free survival in newly diagnosed multiple myeloma studies: a meta-analysis. Clin Lymphoma Myeloma Leuk. 2020;20(1):e30-e37.
- Munshi NC, Avet-Loiseau H, Anderson KC, et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 2020;4(23):5988-5999.
- Lahuerta J-J, Paiva B, Vidriales M-B, et al. Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J Clin Oncol. 2017;35(25):2900-2910.
- Martinez-Lopez J, Wong SW, Shah N, et al. Clinical value of measurable residual disease testing for assessing depth, duration, and direction of response in multiple myeloma. Blood Adv. 2020;4(14):3295-3301.
- Landgren O, Iskander K. Modern multiple myeloma therapy: deep, sustained treatment response and good clinical outcomes. J Intern Med. 2017;281(4):365-382.
- Anderson KC, Auclair D, Adam SJ, et al. Minimal residual disease in myeloma: application for clinical care and new drug registration. Clin Cancer Res. 2021;27:5195-5212.
- Attal M, Lauwers-Cances V, Hulin C, et al. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2017;376(14):1311-1320.
- Durie BGM, Hoering A, Abidi MH, et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet. 2017;389(10068):519-527.
- Wolf J, Fonseca R, Muffly L. Clinical actionability of measurable residual disease (MRD) assessment in the management of patients with hematologic malignancies: a case-based monograph. Clin Adv Hematol Oncol. 2020;18(3)(suppl 9):1-16.
- Martinez-Lopez J, Alonso R, Wong SW, et al. Making clinical decisions based on measurable residual disease improves the outcome in multiple myeloma. J Hematol Oncol. 2021;14(1):126.